| What is Chlamydia? |
| How do you get Chlamydia? |
| Who is at risk of contracting Chlamydia? |
| Chlamydia symptoms |
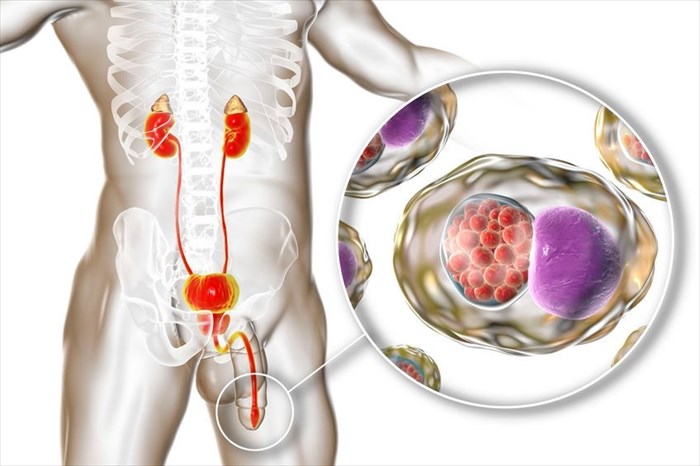
| Chlamydia in men |
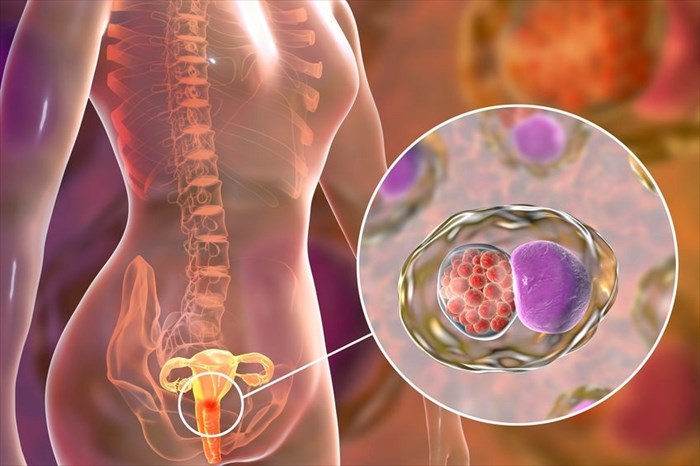
| Chlamydia in women |
| Chlamydia syndromes common to both men and women |
| Chlamydia in newborns |
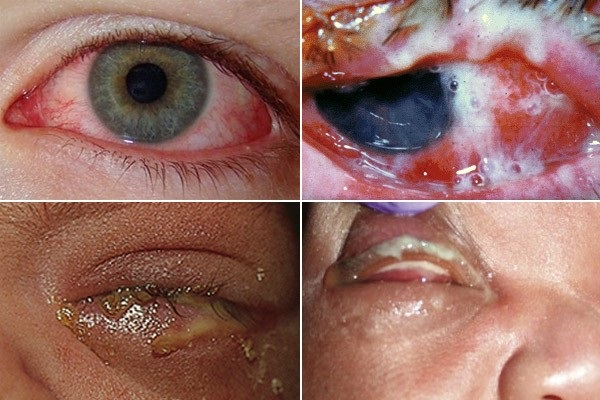
| What does Chlamydia look like? |
| How is Chlamydia diagnosed? |
| Chlamydia tests |
| Chlamydia Treatment |
| Home remedies for Chlamydia |
| Chlamydia Prevention |
| Chlamydia FAQs |
What is Chlamydia?
Chlamydia, sometimes referred to as 'the clam' is among the most common sexually transmitted infections. It is caused by the bacterium Chlamydia trachomatis (C. trachomatis).
Ludwig Halberstädter and Stanislaus von Prowazek discovered the disease in the year 19071. The genus part of the name, Chlamydia, originates from the Greek word 'chlamys', meaning 'cloak'. The word 'trachomatis' which describes the species is also Greek and means 'rough' or 'harsh'.
Both men and women may become infected with Chlamydia, and it is estimated that approximately 105.7 million new cases occur annually worldwide2.
Chlamydia is often called a 'silent STI' as the majority of infected people don't exhibit symptoms and are therefore not even aware that the infection is present. Even when signs and symptoms do occur, they may be so mild that they pass unnoticed. This not only increases the risk of transmission but also means that the previously quoted infection figures are probably largely underestimated.
If left untreated, Chlamydia can cause serious health problems, particularly in women.
How do you get Chlamydia?
Chlamydia is spread through engaging in vaginal, anal, oral sex with an infected person. The infection can be transmitted even if a male partner does not ejaculate (cum).
Pregnant women with untreated Chlamydia can also pass the infection to their babies during delivery. Chlamydia in newborns can manifest as severe eye infections (conjunctivitis) or lung infections.
Who is at risk of contracting Chlamydia?
Any sexually active person engaging in unprotected sexual intercourse (vaginal, anal or oral sex) is at risk of contracting Chlamydia. Some groups are at a higher risk due to various biological, behavioural and cultural factors common to them. These include engaging in unprotected sex (i.e. not using condoms consistently) and moving quickly from one monogamous relationship to the next.
These groups include:
- Young people (almost two-thirds of chlamydia infections occur in those between the ages of 15 and 24 years old2)
- Men who have sex with men3
- Women who have sex with women4
- Those who have previously had Chlamydia. This is often because these individuals are at higher risk of being reinfected by an untreated sexual partner or a new one moving within the same network as the previous one.
- Those with a history of other sexually transmitted infections (STIs)
- Those who do not practice safe sex consistently
- Unborn babies of mother's with untreated chlamydial infections
Chlamydia symptoms
Most of those infected with Chlamydia often do not experience any signs or symptoms of infection or these may be so mild that they are easily overlooked. On rarer occasions when symptoms do occur, they may include the following:
Chlamydia symptoms in men
- Pain when urinating
- Lower abdominal pain
- Abnormal discharge from the penis (this is usually white, cloudy or watery)
- Testicular pain and/or swelling
- Inflamed rectum
Chlamydia symptoms in women
- Painful urination
- Lower back pain
- Lower abdominal pain
- Abnormal vaginal discharge
- Pain during sex
- Bleeding after sex
- Bleeding between menstrual periods
- Inflamed rectum
In some rarer cases, the C. trachomatis bacterium can cause various clinical syndromes in both men and women. The term 'clinical syndromes' refers to a set of medical signs and symptoms and collection of diseases that aren't connected but are explained by identifying the underlying cause.
These are as follows:
Chlamydia in men
Chlamydia (C. trachomatis) is often the underlying cause of several conditions in men. These include:
- Urogenital infections (i.e. infections of the urinary and genital organs)
- Urethritis5 (inflammation of the urethra – the tube that carries urine from the bladder to outside of the body): Pain when urinating is usually the primary symptom associated with this condition. A clear, mucus-like or watery discharge may also be experienced but may be so slight that it is only noticeable when it stains underwear.
- Epididymitis (inflammation of the epididymis – the coiled tube located at the back of the testicles that stores and carries sperm): C. trachomatis is a common cause of this condition in men younger than the age of 35. Signs and symptoms include a tender or painful testicle (one, not both), a fluid-filled sac (hydrocele) that causes swelling of the scrotum (the pouch of skin that contains the testes) and/or swelling of the epididymis that can be felt upon physical examination.
- Proctitis: Chlamydial proctitis involves the inflammation of the inner lining of the rectum (the lower part of the large intestine that ends in the anus).
Chlamydia in women
C. trachomatis bacterium may cause several clinical syndromes in women6. The cervix (the cylinder-shaped neck of tissue that connects the vagina and uterus) is most commonly affected by Chlamydia. Some women may experience an infection of the urethra. This is the tube connecting the bladder to the outside of the body for the removal of urine.
Untreated cervical infections can move upwards, causing pelvic inflammatory disease (PID), which may lead to chronic pain and infertility. Pregnant women with genital Chlamydia are also at increased risk of experiencing pregnancy complications.
Syndromes that may occur as a result of underlying chlamydia infection in women include:
- Cervicitis (inflammation of the cervix): The majority of women with this condition do not have symptoms. For this reason, it is generally recommended that young, sexually active women undergo annual pap smear tests. These tests can also include samples taken for Gonorrhoea and chlamydia testing. When symptoms do occur, they are usually non-specific and include abnormal vaginal discharge, bleeding in between menstrual periods or after sex7.
- Dysuria-pyuria syndrome due to urethritis (inflammation of the urethra – the tube that carries urine from the bladder to outside of the body): Chlamydial infection of the female urethra occurs in around 25% of those infected. When this type of infection occurs, women generally report symptoms similar to that of a urinary tract infection (UTI) such as frequent, difficult or painful urination (dysuria). When urine is tested pus is often present (pyuria), but no organisms are evident.
- Pelvic inflammatory disease (PID): In a small percentage of chlamydia cases (between 2 to 4.5%)8,9. C. trachomatis can move up the reproductive tract and cause pelvic inflammatory disease. PID is an infection of the female upper reproductive tract including the ovaries, fallopian tubes, endometrium (the innermost lining of the uterus) and pelvic peritoneum (the membrane that lines the pelvic cavity)10. PID symptoms include severe pelvic pain, fever, nausea and abnormal vaginal bleeding between menstrual periods. If left untreated, it can cause several complications, including chronic pelvic pain, ectopic pregnancy, and infertility.
- Perihepatitis (Fitzhugh-Curtis syndrome): Some women with chlamydial infections may develop perihepatitis. This refers to inflammation of the liver capsule (i.e. the layers of connective tissue that cover the liver) and the lining of the peritoneum (the membrane that lines the abdominal cavity). This syndrome is more common in women suffering from pelvic inflammatory disease. It is associated with pain in the right upper area of the abdomen and can be associated with sharp chest pain.
Chlamydia syndromes common to both men and women
In some instances, Chlamydia may be the underlying cause of the following syndromes in both men and women:
- Conjunctivitis: Variations of the chlamydia trachomatis bacteria that cause genital infections can also affect one or both eyes, specifically the conjunctiva. The conjunctiva is the thin, transparent membrane that covers part of the front surface of the eyes and the inner surface of the eyelids. The infection is transmitted by touching infected genital secretions and then touching the eyes. It is generally more common in women than men11. Symptoms range from acute to severe and can include red/pink eyes, itching, swelling, mucous discharge that causes crusting of the eyelashes and the eyelids sticking together, tearing, light sensitivity, the feeling of having something in the eye, blurred vision.
- Pharyngitis: In some instances, C. trachomatis bacteria has been found in throats of men and women who have had oral sex with an infected partner. In rare cases, this may cause pharyngitis. This condition is caused by inflammation of the mucous membranes of the oropharynx that causes a sore, red throat.
Chlamydia in newborns
Pregnant women with active, untreated chlamydia infections may infect their babies with C. trachomatis during vaginal delivery. While delivery via c-section does carry a reduced risk of infection, transmission to the infant may still occur.
When a baby is infected with Chlamydia during delivery, he or she may have no symptoms, or the infection may manifest as eye inflammation (conjunctivitis) and/or pneumonia.
Conjunctivitis
Conjunctivitis occurs in between 30% to 50% of infants infected with chlamydia12. This condition is often referred to as inclusion conjunctivitis of the newborn (ICN)or inclusion blennorrhea. The symptoms usually occur between 5 and 14 days after delivery, although they may be noticeable slightly earlier in premature babies.
Inclusion conjunctivitis of the newborn (ICN) symptoms include:
- Noticeable swelling of the eyelids
- Red, thickened conjunctiva (i.e. the layer that covers the front of the eye and eyelids)
- A layer may form from the infectious secretions and stick to the conjunctiva
- A bloody discharge from the eye
With treatment, ICN usually resolves without causing long-term issues. If, however, the infection remains untreated for months, this can cause scarring and damage to the eye.
Pneumonia
Pneumonia caused by a chlamydial infection of the newborn is referred to as Chlamydia pneumoniae. Research shows that this type of infection occurs in 5 to 30% of infected newborns13. Approximately half of these infants also had conjunctivitis.
Pneumonia caused by C. trachomatis is usually evident in infected babies between 4 and 12 weeks of age, although all show symptoms before 8 weeks. Upper respiratory tract infections may be apparent from 2 weeks onwards.
Symptoms of Chlamydial pneumoniae in infants include:
- Cough
- Nasal congestion (with or without discharge)
- Intermittent breathing issues
What does Chlamydia look like?
Since chlamydial infections are often asymptomatic, it may not be possible to spot these. When symptoms are evident, the most obvious sign is abnormal discharge from the penis or vagina.
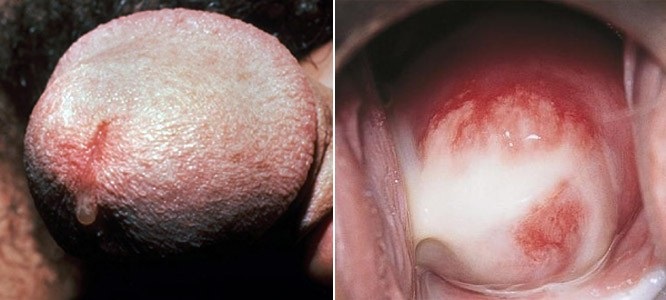
Left: Chlamydia cervicitis as seen during Pap smear (image credit: SOA Amsterdam)
Chlamydia may also cause conjunctivitis, in adults due to contact with infected fluids and in infants due to infection being passed from their mothers during delivery.
How is Chlamydia diagnosed?
Since people infected with Chlamydia often show no signs or symptoms, many don't even know they have it. For this reason, it usually remains undiagnosed until syndromes develop that lead to signs and symptoms that may point to the presence of Chlamydia as the underlying cause.
In women, however, the infection may be picked up during routine gynecological examinations and testing before these syndromes develop.
Men or women who feel they may have inadvertently been exposed to an STD by having unprotected sex should consult with their regular healthcare professional.
In babies born to mothers with untreated chlamydia infections, tests will be run to confirm whether or not they are infected with the disease.
Chlamydia tests
To diagnose Chlamydia, a doctor will generally order one of several tests. The timeline for chlamydia testing is one to two weeks after initial exposure. These tests may include:
- Nucleic acid amplification (NAAT) – This type of test analyses samples from endocervical or vaginal swabs in women, urethral swabs in men, or first catch urine samples (i.e. 20 – 30 ml of urine collected as one begins to urinate without pre-cleansing the genital area) or rectal swabs from both sexes. This type of test identifies small amounts of RNA and DNA in samples and can thus detect the bacterium (Chlamydia trachomatis).
- XPert CT/NGassay – While Chlamydia and Gonorrhoea are two distinct STIs, they often occur together. This rapid test detects and differentiates between Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) to confirm if one, or both infections are present and can yield results within 90 minutes.
Things to tell your doctor and be aware of before having a chlamydia test
It is advisable to inform your doctor if you have engaged in oral or anal sex. This is because the throat or anus/rectum may be infected even when vaginal and urine test samples are negative. A doctor should also be notified if antibiotics are being used at the time of testing.
Women should avoid vaginal creams and douches for at least 24 hours before testing.
Self-ordered chlamydia testing
For some, the thought of seeing a doctor about a possible sexually transmitted infection is extremely embarrassing. While this should not be the case as STDs are widespread nowadays, rather than avoiding the doctor and not getting treated, alternative testing options do exist.
Ordering 100% confidential chlamydia tests online
Some reputable providers offer 100% confidential testing with samples taken by trained professionals at local clinics as required. These types of tests are often more accurate than the self-collected samples as there is less room for error in the collection when administered by trained professionals.
These types of tests can be ordered and paid for online. All of the paperwork is completed at home and uploaded. Then all that remains is popping into a local clinic to give the required sample. This method is not only quick and easy but may also be far less embarrassing. This is because the clinical staff in attendance don't know the reason you're there, only which samples they need to take.
Results are made available either online through a personal dashboard or via e-mail once laboratory testing is complete. An online doctor's consultation may also be purchased to help you interpret the results and to prescribe treatment and/or counselling should this be necessary.
At home chlamydia test kits
Alternatively, an at-home Chlamydia test may be used. A Chlamydia test kit is ordered online and received via courier. Samples are taken according to a detailed set of instructions, packaged and sent back for laboratory testing. These tests are highly accurate, sensitive and reliable provided the instructions are followed. Learn more about these types of at home STD tests here.
Results are available within a few days of testing, either online or via e-mail. If required, a fee for an online or telephonic doctor's call can be paid to assist with the interpretation of the results or to secure a prescription for treatment should this be necessary.
Chlamydia test results
The following may cause infections similar to Chlamydia:
- N. gonorrhoeae, the bacterium that causes Gonorrhoea infection
- Trichomonas vaginalis, the parasite that causes trichomoniasis (trich)
- Mycoplasma genitalium
As such, if a test is negative for Chlamydia, a doctor may consider further STD testing to identify whether the infection present is caused by one of these.
Chlamydia treatment
Can Chlamydia be cured?
Chlamydia is one of the sexually transmitted infections that can be cured with the use of medication.
However, being cured of Chlamydia does not make you immune to the infection. You can become reinfected if you have unprotected sex with an infected person. Clinical studies show a reinfection rate of 13.9% in women14 and 11.3% in men15.
Chlamydia treatment aims to:
- Prevent complications
- Lower the risk of transmission from the infected person to others
- Resolve any symptoms experienced as a result of the infection (if these are present)
Treatment of uncomplicated chlamydia infections
Once a chlamydia infection has been confirmed through a positive test result, a doctor will generally prescribe an antibiotic. These may include azithromycin (1 gram) as a single dose therapy or doxycycline for an extended period (100mg taken twice daily for 7 days). Both the infected person and their sexual partner should take this medication to prevent reinfection.
It is essential to take these antibiotics as directed, and where applicable, finish the course. Stopping antibiotics prematurely can cause them to be ineffective, lowering cure rates.
While the above are generally the preferred first-line treatment options, alternatives may be considered by your prescribing doctor in certain circumstances. These may include:
- Ofloxacin
- Levofloxacin
- Erythromycin base
- Erythromycin ethyl succinate
- Penicillin
Treatment is the same for both HIV-positive and HIV-negative individuals.
Sex after being treated for Chlamydia
Sexual activity should be avoided for seven days following the commencement of treatment. Waiting 7 days after chlamydia treatment is necessary to give the antibiotics time to work and clear up the infection. Provided symptoms resolve and both partners have been treated, sexual activity may resume thereafter.
If symptoms persist, this may be indicative of the presence of another type of sexually transmitted infection or reinfection with Chlamydia. In these instances, sexual abstinence is recommended until the cause can be identified.
Follow-up testing for Chlamydia
Repeat testing will be required three months after treatment has taken place. This is to ensure that the infection has been eradicated and no reinfection has taken place.
Treatment for those with Chlamydia and Gonorrhoea
In those infected with both Chlamydia and Gonorrhoea, a doctor will prescribe appropriate medications as the above alone will not be sufficient to treat Gonorrhoea. You can learn more about Gonorrhea and its treatment options here.
Treating Chlamydia during pregnancy
During pregnancy, alternative treatment considerations may be required.
It is necessary to treat chlamydial infections in pregnant women to prevent them passing C. trachomatis to their babies during delivery. Generally, a single dose antibiotic will be prescribed (azithromycin or similar) and if this cannot be tolerated alternatives may be recommended.
Doxycycline, levofloxacin, ofloxacin, and erythromycin should not be used in pregnancy or when a woman is breastfeeding. Follow-ups and repeat testing approximately 3 weeks after treatment has been completed will be necessary. This is because chlamydia cure rates in pregnant women are generally lower than non-pregnant ones. Further follow-up is required at around three months.
Treatment of babies infected with Chlamydia during delivery
In infants, the decision regarding the type of treatment and when to commence, it will depend on the type of infection present.
Conjunctivitis will be treated after a positive diagnostic test. Pneumonia will be treated based on the symptoms until diagnostic tests offer confirmation that the illness is caused by C. trachomatis.
Antibiotics (often erythromycin or azithromycin) will be administered accordingly. It is important to note that erythromycin or azithromycin are associated with an increased risk of infantile hypertrophic pyloric stenosis (IHPS). This is more prevalent when these medications are administered to infants younger than two weeks of age. IHPS is a condition in which the opening between the stomach and small intestine thickens. This thickening can cause a complete obstruction that leads to forceful vomiting. A doctor will discuss these risks along with what to look out for in cases where he/she deems this necessary.
In most cases, chlamydial infections are effectively treated with these antibiotics. Follow-ups to confirm that the treatment has been effective are necessary.
Home remedies for Chlamydia
A quick online search reveals some home remedies for Chlamydia, with many claiming these are powerful chlamydia cures.
While some substances recommended may offer antibacterial properties and aid in symptom relief, the only scientifically proven cure for Chlamydia is antibiotics. Chlamydia complications are serious, and this infection may cause chronic health issues and even infertility, as such, prompt, appropriate medical treatment is necessary to prevent these. Relying on non-medical home remedies is dangerous and should not be considered as a form of treatment for Chlamydia.
In addition, it is important to discuss taking any of these supplements with your doctor. This is because certain supplements can interact with antibiotics and interfere with their potency and effectiveness.
Here's the truth about the various chlamydia home remedy claims:
- Aloe vera: Due to aloe vera's antibacterial properties, some claim that it can be used to treat Chlamydia. Studies on its effects in humans are still ongoing16.
- Chlamydia diet: There are some claims that you can get rid of Chlamydia fast by following a specialised diet. The proposed eating plans consist particularly of fruit, vegetables and herbs while supplementing with probiotics. Eating well helps to boost your immune system and taking probiotics while you take antibiotics to treat Chlamydia can help to protect your gut health. However, diet and probiotics alone cannot cure the infection.
- Echinacea: Echinacea extract has immune-boosting properties. As such, it can help the body fight off certain bacterial and viral infections. There is, however, no scientific evidence to prove that it can treat a chlamydia infection.
- Garlic: A popular home remedy for almost every ailment, garlic's antibacterial and anti-inflammatory properties are widely touted. While these do have bacteria-fighting abilities, garlic does not destroy the bacteria that cause Chlamydia. It may, however, be beneficial when taken along with antibiotics to treat Chlamydia as it prevents the growth of yeast. Yeast overgrowth can lead to the development of yeast infections, and this is often associated with antibiotic use.
- Goldenseal: This herb is linked to the treatment of a variety of conditions, including Gonorrhea and Chlamydia. While some preliminary evidence shows that it has antibacterial properties17, there is nothing to support its use in treating sexually transmitted infections like Chlamydia.
- Olive tree extract: Olive tree extract contains Oleuropein, a compound known for its anti-inflammatory, antiviral and antimicrobial properties. While this supplement has many proven health benefits, curing Chlamydia is not one of them.
- Turmeric: Another health benefit powerhouse, turmeric contains curcumin which has potent anti-inflammatory and antioxidant properties. Some studies show promising results when using turmeric to treat Chlamydia in a lab setting. Nevertheless, at present, there isn't enough evidence to support using turmeric as a chlamydia cure in humans18,19.
Chlamydia Prevention
The only way to completely prevent chlamydia infection is to abstain from sexual intercourse. If that's not an option:
- Use condoms: Both the latex male condom and polyurethane female condom can provide effective barriers against infection during sexual intercourse. They cannot eliminate the risk of contracting the infection but can reduce it.
- Limit your number of partners: Having sex with multiple partners increases your risk of infection not only with Chlamydia but all STIs.
- Avoid douching: Douching to prevent STIs is ineffective and reduces populations of good bacteria necessary to maintain a healthy balance within the vagina. When these are no longer present, the risk of infection rises.
- Get tested regularly: If you're sexually active and especially if you have multiple partners, chat to your doctor about getting screened for Chlamydia and other STIs.
Chlamydia FAQs
Is Chlamydia curable?
Yes. Chlamydia is curable with the help of antibiotics.
Can you get Chlamydia from kissing?
No. You can't catch Chlamydia from kissing, hugging, sharing utensils, glasses or a toilet with an infected person. Chlamydia is transmitted through unprotected oral, vaginal or anal sex with an infected person.
Can you get Chlamydia from oral sex?
Yes. Chlamydia can be transmitted through oral sex with an infected person.
Can you get Chlamydia without being sexually active?
Some infants are infected with C. trachomatis, the bacteria that causes Chlamydia at birth. Apart from this, you cannot become infected without performing a sexual act. Penetrative sex is not the only way a person becomes infected. You may also contract Chlamydia through contact with an infected person's sexual fluids (for example if your genitals touch).
Are Chlamydia and trichomoniasis the same?
Chlamydia and trichomoniasis are both sexually transmitted infections, but they are not the same thing. Chlamydia is caused by the C. trachomatis bacteria while trichomoniasis is caused by a parasite (Trichomonas vaginalis).
Both may show similar symptoms or no symptoms at all, so testing for these STIs is the only way to confirm whether or not you have one, or both of them.
Why are Chlamydia and Gonorrhoea tested for together?
Chlamydia and Gonorrhoea are referred to as co-existing infections. This is because infected individuals often have both diseases at the same time. When symptoms of these infections do occur, they are often similar. As such, it's vital to test for these together.
How does Chlamydia affect your period?
Chlamydia may cause abnormal spotting or bleeding in between menstrual periods. According to Oxford University Research, the presence of a sexually transmitted infection like Chlamydia, doubled the likelihood of the woman in their study reporting adverse premenstural symptoms. These include headaches, cramps and sadness towards the end of their cycle, as well as heightened sensitivity throughout it20.
What happens when Chlamydia goes untreated?
If left untreated, Chlamydia can cause serious complications, particularly in women. Chlamydia can spread upwards from the cervix to the uterus and fallopian tubes (i.e. the tubes that connect the ovaries to the uterus and carry the fertilised egg to the womb during pregnancy). This infection can cause pelvic inflammatory disease (PID), which can result in fertility issues and permanent damage to the reproductive system.
Health issues and complications in men are rare. Infection may spread to the tubes that carry sperm from the testicles, and this may cause pain and fever, but it rarely leads to fertility issues.
Why are women more affected by Chlamydia?
Men and women get Chlamydia in almost equal numbers. However, they are not affected equally by this disease. Women generally have a higher risk of contracting STIs than men21 due to their anatomic makeup which makes them more susceptible to infection.
The vaginal lining is thinner and more delicate than the skin on the penis, making it easier for bacteria and viruses to enter. The moist vaginal tissues are an ideal environment for bacterial growth. Also, women are less likely than men to experience symptoms that lead to care and treatment.
When symptoms do occur, they can easily be mistaken for something else. For example, an abnormal vaginal discharge along with vaginal itching and burning may be mistaken for a vaginal yeast infection. When burning occurs along with urination, a urinary tract infection (UTI) may be thought to be the cause. In men, discharge or burning are often noticed immediately.
Also, the complications that arise in infected women are more severe than those that occur in men.
What happens if Chlamydia comes back?
It is possible to be reinfected with Chlamydia even after being given the 'all clear' following treatment. This may occur when you have unprotected anal, oral or vaginal sex with an infected person.
In this event, it will be necessary to be re-tested and re-treated with follow-up testing. Your partner/s should also be tested and treated. You should also wait 7 days for the medication to take effect before returning to sexual activity. This helps to ensure that infection does not recur.
References
1. Ripa K. Microbiological diagnosis of Chlamydia trachomatis infection. Infection. 1982;10(S1):S19-S24. doi:10.1007/bf01640710
2. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/75181/9789241503839_eng.pdf;jsessionid=ECB284232646748466396E3CE09E3E4B?sequence=1. Published 2008. Accessed September 18, 2019.
3. Kent C, Chaw J, Wong W et al. Prevalence of Rectal, Urethral, and Pharyngeal Chlamydia and Gonorrhea Detected in 2 Clinical Settings among Men Who Have Sex with Men: San Francisco, California, 2003. Clinical Infectious Diseases. 2005;41(1):67-74. doi:10.1086/430704
4. Singh D, Fine D, Marrazzo J. Chlamydia trachomatis Infection Among Women Reporting Sexual Activity With Women Screened in Family Planning Clinics in the Pacific Northwest, 1997 to 2005. Am J Public Health. 2011;101(7):1284-1290. doi:10.2105/ajph.2009.169631
5. O'Connell C, Ferone M. Chlamydia trachomatis Genital Infections. Microbial Cell. 2016;3(9):390-403. doi:10.15698/mic2016.09.525
6. Witkin S, Minis E, Athanasiou A, Leizer J, Linhares I. Chlamydia trachomatis: the Persistent Pathogen. Clinical and Vaccine Immunology. 2017;24(10). doi:10.1128/cvi.00203-17
7. Allen M. Identifying acute cervicitis in an era of less-frequent routine gynecologic examinations. Journal of the American Academy of Physician Assistants. 2018;31(2):50-53. doi:10.1097/01.jaa.0000530277.12517.69
8. Geisler W, Wang C, Morrison S, Black C, Bandea C, Hook E. The Natural History of Untreated Chlamydia trachomatis Infection in the Interval Between Screening and Returning for Treatment. Sex Transm Dis. 2008;35(2):119-123. doi:10.1097/olq.0b013e318151497d
9. Bachmann L, Richey C, Waites K, Schwebke J, Hook E. Patterns of Chlamydia trachomatis Testing and Follow-Up at a University Hospital Medical Center. Sex Transm Dis. 1999;26(9):496-499. doi:10.1097/00007435-199910000-00002
10. Trent M, Das B, Ronda J. Pelvic inflammatory disease: improving awareness, prevention, and treatment. Infect Drug Resist. 2016;Volume 9:191-197. doi:10.2147/idr.s91260
11. Yang E, Oetting T. EyeRounds.org: Adult-Chlamydial-Conjunctivitis-Red-Eyes-Chronic. University of Iowa Health Care. https://webeye.ophth.uiowa.edu/eyeforum/cases/68-Adult-Chlamydial-Conjunctivitis-Red-Eyes-Chronic.htm. Published 2007. Accessed October 7, 2019.
12. Zikic A, Schünemann H, Wi T, Lincetto O, Broutet N, Santesso N. Treatment of Neonatal Chlamydial Conjunctivitis: A Systematic Review and Meta-analysis. J Pediatric Infect Dis Soc. 2018;7(3):e107-e115. doi:10.1093/jpids/piy060
13. Chlamydia of the Newborn | Pediatrics Clerkship | The University of Chicago. Pedclerk.bsd.uchicago.edu. https://pedclerk.bsd.uchicago.edu/page/chlamydia-newborn. Accessed October 7, 2019.
14. Hosenfeld C, Workowski K, Berman S et al. Repeat Infection With Chlamydia and Gonorrhea Among Females: A Systematic Review of the Literature. Sex Transm Dis. 2009;36(8):478-489. doi:10.1097/olq.0b013e3181a2a933
15. Fung M, Scott K, Kent C, Klausner J. Chlamydial and gonococcal reinfection among men: a systematic review of data to evaluate the need for re-testing. Sex Transm Infect. 2007;83(4):304-309. doi:10.1136/sti.2006.024059
16. Potroz M, Cho N. Natural Products for the Treatment of Trachoma and Chlamydia trachomatis. Molecules. 2015;20(3):4180-4203. doi:10.3390/molecules20034180
17. Ettefagh K, Burns J, Junio H, Kaatz G, Cech N. Goldenseal (Hydrastis canadensisL.) Extracts Synergistically Enhance the Antibacterial Activity of Berberine via Efflux Pump Inhibition. Planta Med. 2010;77(08):835-840. doi:10.1055/s-0030-1250606
18. Brown M, Potroz M, Teh S, Cho N. Natural Products for the Treatment of Chlamydiaceae Infections. Microorganisms. 2016;4(4):39. doi:10.3390/microorganisms4040039
19. Bhengraj A, Dar S, Talwar G, Mittal A. Potential of a novel polyherbal formulation BASANT for prevention of Chlamydia trachomatis infection. Int J Antimicrob Agents. 2008;32(1):84-88. doi:10.1016/j.ijantimicag.2008.02.010
20. Alvergne A, Vlajic Wheeler M, Högqvist Tabor V. Do sexually transmitted infections exacerbate negative premenstrual symptoms? Insights from digital health. Evol Med Public Health. 2018;2018(1):138-150. doi:10.1093/emph/eoy018
21. Wong T, Singh A, Mann J, Hansen L, McMahon S. Gender Differences in Bacterial STIs in Canada. BMC Womens Health. 2004;4(Suppl 1):S26. doi:10.1186/1472-6874-4-s1-s26