| What is a blood type test |
| When will a blood type test be ordered? |
| Understanding how different blood types are determined |
| Why is knowing your blood type useful? |
| Types of blood type tests |
| Clinical blood type tests |
| Rapid Results and home blood type test kit options |
| Blood type compatibility |
What is a blood type test?
A blood type test also referred to as an ABO blood group test or 'blood typing', determines your ABO blood group and RH (rhesus) type.
Your blood type is a genetic trait that is inherited based on what your parents have passed down to you1, much like your eye and hair colour. It is dictated by the absence or presence of certain proteins (or in some cases, carbohydrates), known as antigens, on the surface of the red blood cells, as well as the antibodies (protective proteins that help to fight off foreign bodies, infection and disease-causing invaders) present in the blood's plasma (the liquid part of the blood without the cells).
When will a blood type test be ordered?
While blood type testing is not generally part of routine medical health screening, a doctor or clinic may order a blood type test:
- In pre-pregnancy counselling for both partners (this is to determine the risk of Rhesus (Rh) incompatibility with a foetus)
- When a pregnancy test is positive (if pre-pregnancy testing was not undertaken)
- Before surgery (or in an emergency situation if time allows) in case you need to receive a blood transfusion or blood components
- If you wish to donate blood
- If you donate an organ, tissue or bone marrow for transplant
- Upon your request
Understanding how different blood types are determined
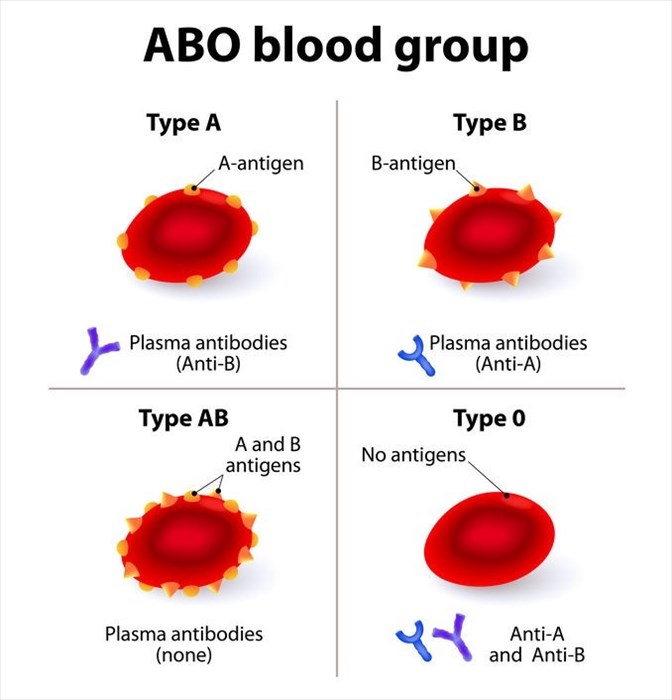
ABO blood typing
The ABO blood group test determines your blood type based on the ABO blood group system. This system is comprised of four major blood groups which are based on the absence or presence of two specific antigens – A and B on the surface of the red blood cells, and the absence or presence of anti-A or anti-B antibodies in the plasma (the liquid part of the blood). To understand this statement is it necessary to understand what antigens and antibodies are and their function:
- Antigens are molecules made up of proteins and/or sugars that are capable of eliciting an immune system response.
- Antibodies (immunoglobins) are y-shaped proteins that fight off foreign invaders in the body (these are referred to as antigens).
Certain blood types have specific red cell antigens that are recognised by the immune system as being native to the body. If an antigen is identified as being 'foreign' these cells will be targeted by the immune system and destroyed. An individual with a certain blood type will thus develop antibodies against the antigens that they don't naturally have.
The blood groups are determined according to these as follow:
| Blood Group | Antigen Present on red blood cells | Antibody present in blood plasma |
| A | A antigen | Anti-B antibody |
| B | B antigen | Anti-A antibody |
| AB | AB antigen | None |
| O | None | Both Anti-A & Anti-B antibodies |
Rhesus (Rh) typing
Another element to blood typing is based on the absence or presence of the Rhesus (RH) factor or D-antigen (RhD) on the surface of the red blood cells. If this antigen is present, your blood is referred to as rhesus positive (Rh+) or 'positive' and if it's not, then your blood type is rhesus negative (Rh-) or 'negative'.
From ABO and Rhesus factor blood typing, the eight blood types are derived as follows:
- A positive (A+)
- A negative (A-)
- B positive (B+)
- B negative (B-)
- AB positive (AB+)
- AB negative (AB-)
- O positive (O+)
- O negative (O-)
Why is knowing your blood type useful?
Prior to surgery or in emergency situations
Knowing your blood type is important prior to surgery and in emergency medical situations where you may have lost a great deal of blood and require a life-saving blood transfusion. In these instances, it is imperative that the correct blood type be given.
With modern testing, transfusions using mismatched blood types (i.e. either blood of a different group or mismatched Rh factor) are exceptionally rare. However, in life-threatening emergencies where substantial blood loss has occurred, time is of the essence in administering a transfusion.
While blood type testing will generally always be done in instances where a transfusion is required, this is not always possible. Sometimes access to testing facilities is not immediately at hand, or there is insufficient time available to order a blood type test and cross-match in order to ensure accurate blood type matching before treatment is administered.
In these situations, O negative blood is generally regarded as the safest blood type to transfuse. This is because this blood type does not have A, B or Rh antigens and therefore the recipients A, B and Rh antibodies will not attack the donor blood. As such, people with O negative blood were once referred to as 'universal donors' and it was believed they could donate to any blood type.
It has since been established that there may be some risk in giving O negative blood to people with other blood types. So, while it can be done in emergencies, the safest option is to always cross match blood types correctly.
Receiving the wrong blood type may cause a severe, life-threatening reaction known as an ABO incompatibility reaction2. This reaction occurs when the immune system treats the red blood cells of the mismatched blood introduced to the body via a blood transfusion as foreign invaders and develops antibodies to attack and destroy them.
This antigen-antibody reaction not only renders the blood transfusion useless, but also causes an inflammatory response throughout the body. This may lead to shock, fever, low blood pressure, blood clotting throughout the body that clogs the small blood vessels, leading to circulatory collapse, acute kidney injury and even death3,4.
Pregnancy
A baby's blood group and type are determined by inherited traits from its parents. Foetal blood group and type can influence the antibodies the mother's body produces as part of the immune response to foreign bodies in her own body, including that of sperm and even an embryo.
ABO incompatibility in pregnancy
In some instances, issues may arise if a woman with O type blood has a baby with an A, B or AB blood type and the two blood types come into contact with one another during delivery. While relatively rare (generally only occurring in around 1.5 to 2.5% of pregnancies5), when this happens, the A and B antibodies contained in the O type blood attack and destroy the baby's red blood cells, causing haemolytic disease of the foetus and newborn (HFDN). This condition usually presents as jaundice (yellowing of the skin, whites of the eyes and mucous membranes) in the newborn.
ABO incompatibility is screened for during the early stages of pregnancy, usually at the first prenatal visit. If antibodies are detected, follow-up tests will be conducted, and treatment will begin.
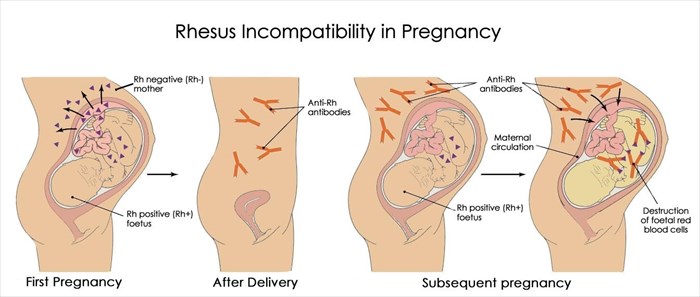
Rhesus incompatibility in pregnancy
During pregnancy, issues may arise if an Rh negative mother carries an Rh positive child. This is referred to as rhesus (Rh) incompatibility. It is generally quite rare, affecting only around 1% of pregnancies.
While a mother's blood does not usually come into contact with that of her unborn child during pregnancy, this may occur during certain invasive tests, in instances of bleeding or abdominal trauma or during delivery.
In such cases, the body may produce antibodies in reaction to exposure to the baby's red blood cells. These antibodies will target and attack the baby's red blood cells perceived to be foreign invaders in an attempt to neutralise the threat. This is known as Rhesus disease or Haemolytic disease of the foetus and newborn (HFDN) and usually causes the baby to become anaemic and develop jaundice6.
While this is often not a problem in the first pregnancy, it may cause an issue in a subsequent one. If the next baby is also Rh positive, the Rh antibodies that the mother's body produced in response to the previous pregnancy would cross the placenta and damage the baby's red blood cells, causing anaemia which could be life-threatening.
It is for this reason that your doctor will recommend a blood type test with Rh factor screening once pregnancy is confirmed. If you are Rh negative, he/she may recommend an additional antibody screen during your first trimester, repeated at week 28 of pregnancy and again at the time of delivery. This test will determine whether antibodies to Rh positive blood have developed. If they have not, Rh immune globulin (marketed under the brand name RhoGAM) will be injected to prevent this from happening in future.
If both you and your baby are Rh negative (this will usually only be established once a baby is born), no additional treatment will be required. If, however, your baby is born Rh positive, an additional injection of Rh immune globulin (RhoGAM) will be administered within 72 hours of delivery.
If you are Rh negative you may also be given this type of injection in any instance where your blood may come into contact with your baby's blood, including during a miscarriage, abortion, ectopic pregnancy (where fertilised eggs implant outside of the uterus), during prenatal diagnostic tests, if bleeding or trauma occurs, or if a baby is manually rotated from a breech position (i.e. if a baby is not head down and needs to be turned) during labour.
If the antibody screen shows that you are producing antibodies, the administration of Rh immune globulin will not be effective. As such, both you and your baby will be carefully monitored, and he/she may require a blood transfusion via the umbilical cord during pregnancy or once he/she is delivered.
Donating blood, organs and tissue
When it comes to transfusion medicine, it is vital that a person requiring a blood transfusion only receives blood cells that are compatible with their own blood type in order to avoid a potentially life-threatening incompatibility reaction. In those receiving a blood plasma transfusion (the liquid part of blood without the cells) it is important that they are not transfused with plasma which contains antibodies that will destroy their own red blood cells.
As such, all blood donors and blood transfusion recipients undergo blood type testing before transfusions take place.
One of the first steps in organ transplants is to determine the compatibility of the donor and recipient's blood types. Matching or compatible ABO blood types are necessary to lower the risk of organ rejection. If these are not compatible, direct organ donation is not possible.
Types of blood type tests
There are currently two types of blood type testing available:
- Clinically administered blood type tests: This is the most common method of blood type testing. These tests are administered by a doctor or nurse and blood samples are sent to a laboratory for analysis. Analysis usually involves a 2-step testing approach including a forward blood group testing which identifies the antigens (A and B) on the red blood cells, and reverse grouping which identifies the specific antibodies present in the plasma. Analysis usually takes anywhere between 5 and 20 minutes to complete. Once this has been completed, the results are made available to the doctor and/or patient.
- Rapid results blood type test / home blood type test kit: Due to advancements in modern medicine, rapid results blood type tests are also possible. These types of tests are generally used by first responders and the military for clinical purposes, while the blood type test kits for home use can be used by the general public for informational purposes.
Clinical blood type tests
Where do you do a blood type test?
Blood type tests are conducted in a laboratory. Your doctor may draw blood in his/her office, a nurse may take blood at a clinic or hospital or you may be sent directly to the lab for the blood draw to take place.
How do I prepare for a blood type test?
Blood type tests do not require any prior preparation. You can generally eat, drink and take your medication as usual unless otherwise indicated by your healthcare provider. You should, however, always ensure that your doctor is aware of all of the medications, both over-the-counter and prescription that you are taking, as well as any herbs, vitamins, supplements or illicit drugs you may be taking before any blood test is done.
Collection of blood sample
In order to have a blood type test, a blood sample will be required. This is obtained as follows:
Infants
In newborn infants, blood make be taken from the umbilical cord or from a heel stick.
Babies, children and adults
In babies, children and adults, a sample will generally be drawn from a vein in the arm (most commonly inside the elbow) or the back of the hand when conducted in a medical setting.
The doctor or nurse taking the blood will place a band around the upper arm to apply pressure and cause the vein from which the blood will be drawn to swell. The area from which the blood will be drawn will be cleaned with a disinfectant wipe. A needle will be inserted into the vein and the blood drawn will be collected in the attached tube. The band around the arm will be loosened to restore blood circulation and once the blood required is collected the needle will be removed and gauze or cotton wool and a plaster applied.
This type of test is not painful, you may feel a slight sting when the needle is inserted, but this is generally mild. Slight bruising may occur in the area from which the blood was drawn, and this will resolve on its own within a few days.
Risks
There is minimal risk associated with having blood drawn. It may cause minor discomfort in some and none in others. This is because vein sizes differ from one person to the next as well as from one side of the body to the other.
While rare, the following risks may be associated with blood draws in some people:
- Feeling lightheaded
- Fainting
- Difficulty in locating a vein, resulting in multiple attempts to draw blood
- Excessive bleeding
- Haematoma (accumulation of blood beneath the skin)
- Infection (this is a slight risk whenever the skin is broken)
Analysis of blood sample
The blood sample collected will be tested and analysed to determine blood type as follows:
ABO typing
In ABO typing, your blood sample will be mixed with sera containing antibodies against type A and B blood (anti-sera). The samples will be analysed to determine whether or not the red blood cells stick together (agglutinate). If they do, it means your blood reacted to one of the antibodies present. Your blood type matches whatever antibody caused the clumping. So, for example, if your blood clumps in the presence of the anti-B antibodies, it is type B and carries the B antigen.
| If your blood clumps (agglutinates) in: | You are blood type: |
| Anti-A, but not Anti-B | A |
| Anti-B, but not Anti-A | B |
| Anti-A and Anti B | AB |
| Neither Anti-A nor Anti-B | O |
The second step in this process is referred to as serum grouping or reverse typing. In this process the blood serum (i.e. the liquid part of your blood without cells) is mixed with confirmed type A and type B blood and the clotting patterns are recorded.
Rhesus (Rh) typing
Rhesus or Rh typing is conducted in a similar manner to ABO typing, although in this test, your blood is tested to see if a Rh factor (RhD) is present on the surface of the red blood cells (RBCs). A drop of anti-RH antibodies (Anti-D) will be added to a drop of your blood on a slide. If the blood does not have a rhesus factor present on the surface of the RBCs (i.e. it is Rh negative), it will not clump. If clumping of the blood cells occurs, then it is Rh positive, and the rhesus factor is present.
| If your blood clumps (agglutinates) in: | You are blood type: |
| Anti-D | Rh positive |
Blood type test results
Your result will be sent to your doctor or healthcare provider who will then tell you which ABO blood type you have:
- Type A blood
- Type B blood
- Type AB blood
- Type O blood
In addition, you'll be told whether you have Rh-positive blood or Rh-negative blood. This adds the 'positive' or 'negative' to the above ABO types.
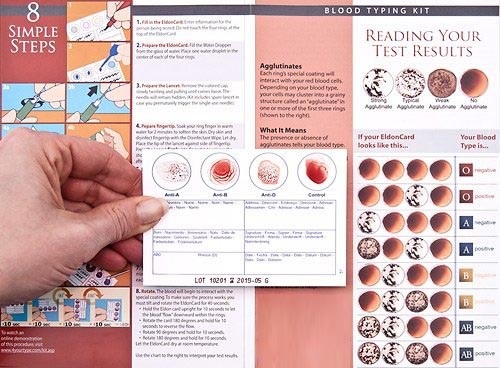
Rapid Results and home blood type test kit options
A number of rapid commercial blood type test kit options are available for ABO and Rh blood typing. Those with health authority approval like the Eldon Card Home Kit 2511 are often used by first responders and the military in emergency situations where there is no access to laboratory testing.
The performance and accuracy of these types of tests does, however, vary according to the product selected, the environmental storage conditions as well as the individual conducting the test. Those with extensive medical training and experience achieve higher accuracy than those with lesser or no experience7,8.
While rapid results blood type test kits are faster and more economical, traditional methods of blood group typing are still considered the most accurate and reliable and are therefore adopted in clinical laboratories9.
Using a home blood type test kit
You can use a rapid blood type test kit to determine your blood type at home but remember that brands with FDA approval are only those intended for use by physicians, clinics and for educational purposes. The results are not approved for reference if a blood transfusion is required and clinical laboratory testing will always be required. As such, if you would like to know your blood type and carry around clinical proof thereof, it is best to ask your doctor or order a blood type test online from a legitimate laboratory, submit your sample (or report to your nearest lab to have it drawn) and send it in for testing.
If you do decide to proceed with a home blood type test for educational purposes, you can purchase these online or at your nearest pharmacy.
How to test your blood type at home
A blood type test kit generally contains:
- Detailed, illustrated instructions A card for the blood test
- Non-reusable sterile automatic lancets
- A plastic dropper (known as a pipette)
- An alcohol prep swab to clean the area you will draw blood from
- Mixing sticks
While these tests are easy to use, they are time sensitive, so it is important to read the instructions in full before you start and follow the steps exactly.
These are as follows:
- Place the card on a clean, dry work surface
- Fill the pipette with saline (or water) and place one drop on the coloured sections at the top of each card.
- Ensure that the mixing sticks are easily accessible
- Use the alcohol prep swab to wipe the finger from which you will take the blood sample.
- Prepare the lancing device by twisting and pulling the safety plug out.
- Put pressure on the finger you will pierce with your other fingers so that the skin firms
- Press the lancing device against the finger until you hear a 'pop'
- Squeeze the punctured area until it forms a blood drop
- Drop the blood onto the mixing stick.
- Apply the blood within one of the circles at the top of the card (try to 'colour in' the whole circle with your blood). Repeat for all circles using a different stick for each one.
- Tilt the card down for a few seconds, then away from you, back to centre, to the right, back to centre and to the left. DO NOT let the blood from each circle run or drip into the adjacent one as this will contaminate the sample and render the results invalid.
- Let the card dry
- Cross match it with the chart included to determine your blood type.
Blood type compatibility
Once you have the results from your blood type test, you will know your blood type. This information will determine the type/s of blood you will be able to safely receive should you need a blood transfusion. If you're a woman your doctor will also be able to advise on whether an incompatibility may occur during pregnancy.
Here's what you need to know:
Red blood cell compatibility
When it comes to blood transfusions, the generally followed principle is that the red blood cells (RBCs) of an identical blood group and Rhesus (Rh) type as those found in the recipient should be transfused. In pregnancy, a foetus with a different but compatible blood type will not cause any issues in either mother or child. The following blood types are compatible10:
| Blood Type | Can receive red blood cells from blood type |
| A | A, O |
| B | B, O |
| O | O |
| AB | AB, A, B, O (all blood types) |
| Rhesus positive (Rh+) | Rh+, Rh- |
| Rhesus negative (Rh-) | Rh- |
It is important to note that in blood transfusions the compatibility between a blood donor's blood and that of the recipient does not always mean that it is an exact match. This is because there are many other antigens in our blood in addition to the major ones mentioned (i.e. A, B and Rh). Many of the minor antigens are not detected during routine blood type screening. If they are not detected and accounted for, they can cause a reaction when receiving a blood transfusion, even if the A, B and Rh antigens have been matched.
For this reason, cross-matching followed by a Coombs test is necessary. Coombs tests help to identify certain antibodies that attack red blood cells11. These tests are ordered before transfusions, except in time-critical emergency situations.
Plasma compatibility
Depending on the blood group, blood plasma will contain either anti-A or anti-B antibodies. Transfusion recipients should only receive plasma that doesn't contain antibodies that will attack their own red blood cells. As such, the following blood types are used when plasma is donated10:
| Blood Type | Can receive plasma from type |
| A | A, AB |
| B | B, AB |
| O | O, A, B, AB (all blood types) |
| AB | AB |
Platelet Compatibility
When a person requires blood platelets (tiny blood cells that aid the body in forming clots to stop bleeding) ABO identical platelets are generally used. In certain circumstances, however, other special requirements may take precedence over ABO group. This will be determined by the doctor overseeing the person's care.
References
1. Garg P. Prevalence of ABO and Rhesus Blood Groups in Blood Donors: A Study from a Tertiary Care Teaching Hospital of Kumaon Region of Uttarakhand. JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH. 2014.doi:10.7860/jcdr/2014/9794.5355
2. Blood Transfusion | UW Health | Madison, WI. UW Health. https://www.uwhealth.org/health/topic/special/blood-transfusion/tc4111.html. Accessed May 28, 2019.
3. Namikawa A, Shibuya Y, Ouchi H, Takahashi H, Furuto Y. A case of ABO-incompatible blood transfusion treated by plasma exchange therapy and continuous hemodiafiltration. CEN Case Rep. 2018;7(1):114-120. doi:10.1007/s13730-018-0307-4
4. Dean L. Blood Groups And Red Cell Antigens. Bethesda (MD): National Center for Biotechnology Information; 2005.
5. ACOG Practice Bulletin No. 192. Obstetrics & Gynecology. 2018;131(3):e82-e90. doi: 10.1097/aog.0000000000002528
6. Rhesus disease. nhs.uk. https://www.nhs.uk/conditions/rhesus-disease/. Accessed May 28, 2019.
7. Bienek D, Charlton D. Accuracy of User-Friendly Blood Typing Kits Tested Under Simulated Military Field Conditions. Mil Med. 2011;176(4):454-460. doi:10.7205/milmed-d-10-00339
8. Bienek D, Perez N. Diagnostic Accuracy of a Point-of-Care Blood Typing Kit Conducted by Potential End Users. Mil Med. 2013;178(5):588-592. doi:10.7205/milmed-d-12-00500
9. Mujahid A, Dickert F. Blood Group Typing: From Classical Strategies to the Application of Synthetic Antibodies Generated by Molecular Imprinting. Sensors. 2015;16(1):51. doi:10.3390/s16010051
10. Blood Transfusion : Blood Groups and Compatibilities. Rch.org.au. https://www.rch.org.au/bloodtrans/about_blood_products/Blood_Groups_and_Compatibilities/. Accessed May 28, 2019.
11. Coombs Antibody Test (Indirect and Direct) | Michigan Medicine. Uofmhealth.org. https://www.uofmhealth.org/health-library/hw44015. Published 2018. Accessed May 28, 2019.
Other Articles of Interest

How does your blood type affect your health?
Research has recently shown that your blood type can have an impact on your health. We explore everything you need to know...

Eating for your blood type – fact or fiction?
When it comes to diets, how much of it is fact and how much is just worthy of being labelled a fad? We take a look at the blood type diet.