Of the numerous inflammatory causes, conjunctivitis is most often classified according to these primary types:
1. Infectious conjunctivitis
There are four forms of conjunctivitis which fall into the infectious category:
Of the four main types of conjunctivitis, fungal and parasitic instances are rarely encountered in the clinical setting, as such, for the purpose of this article, we will focus more on the viral and bacterial causes of the condition.
Viral and bacterial conjunctivitis can be sub-categorised as:
- Hyper-acute (symptoms present quickly – within a few hours of exposure)
- Acute (symptoms present within a few days)
- Chronic (symptoms persist for four weeks or more).
Categories are thus determined according to symptom onset and/or the duration and level of severity experienced.
Viral conjunctivitis
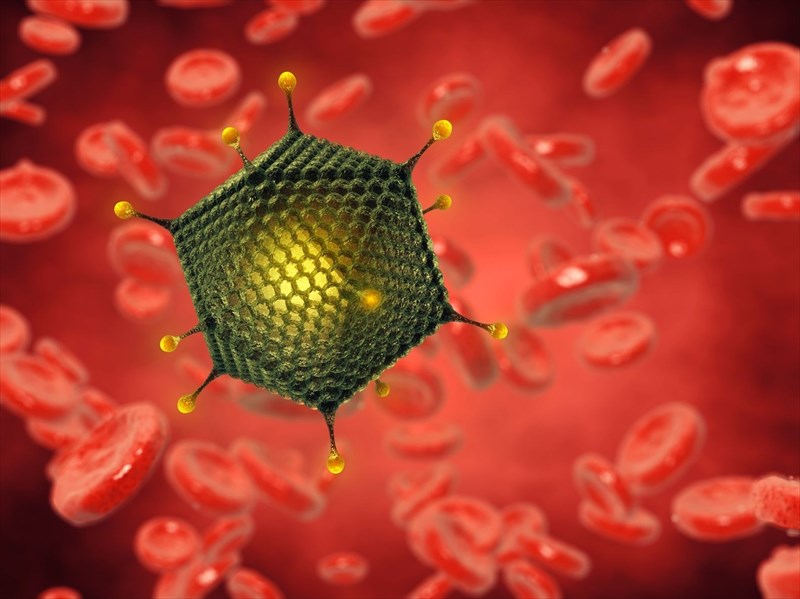
Viral conjunctivitis (pink eye) is highly contagious and the most common type of conjunctivitis. It is triggered by a virus (usually one of the adenoviruses2 - a family of viruses that cause a variety of infections and result in everything from the common cold and respiratory infections to gastroenteritis and neurological diseases).
Other viruses can also cause conjunctivitis include:
- Picornaviruses which result in enteroviruses and the Coxsackie virus (specifically enterovirus 70 and Coxsackie virus A24)
- Poxviruses3 which causes molluscum contagiosum and most commonly affects children
- Herpes Viruses – these viruses present the most problematic forms of conjunctivitis
- Herpes simplex virus (particularly HSV1 which also causes cold sores)
- Varicella-zoster virus (which also causes chickenpox and shingles)
- Epstein-Barr virus which cause a condition known as infectious mononucleosis (mono)
- Rubeola (that results in measles)
- Rubella virus (which causes German measles)
- HIV (human immunodeficiency virus)
When conjunctivitis is caused by adenoviruses and enteroviruses, the condition can spread rapidly through communities and result in conjunctivitis epidemics.
Other viruses, like the poxvirus and the herpes simplex virus, result in skin infections wherein the eye may also become infected if the eyelids are affected. Of all the viruses causing the condition, herpes viruses result in the most serious complications.
Viral conjunctivitis can spread from one eye to the other and also within the body via its own mucous membranes and further affect the nose, throat and lungs, as well as the conjunctiva and tear ducts. A watery discharge is characteristic of infection.
How viral conjunctivitis is spread
Viral conjunctivitis is spread to others through direct and indirect contact as follows:
- Through close personal contact when the liquid that drains from the eye and comes into contact with the hands of the infected person and/or various objects which they use and are then shared with others.
- Via direct hand contact (touching or shaking hands with an infected individual and making contact with the eyes or touching a surface an infected person has made contact with and then the facial area before one’s hands are washed thoroughly).
- Through the infected individual coughing and sneezing which can release the infection into the air via respiratory droplets.
- In swimming pools with insufficient quantities of chlorine.
Bacterial conjunctivitis
Like viral pink eye, bacterial conjunctivitis is also highly contagious although from the reported data, appears to be less common. The specific bacterial causes of conjunctivitis often depend on one’s geographical location (warmer regions have higher incidences) and age and are identified as follows4:
Acute bacterial conjunctivitis:
- Staphylococcus aureus – most common in adults
- Streptococcus pneumoniae – more common in children
- Haemophilus influenzae – more common in children
- Moraxella catarrhalis – more common in children
Hyperacute bacterial conjunctivitis:
- Neisseria gonorrhoeae
- Neisseria meningitidis (rare cause)
- Chlamydia trachomatis
Chronic bacterial conjunctivitis:
- Staphylococcus aureus – most common in adults
- Moraxella lacunata
Transmission of bacterial conjunctivitis infections involves:
- Physical (direct) contact with others
- Inadequate hygiene
- Contact with contaminated objects or substances, such as bedding, facial products or make-up.
- Improperly cleaned contact lenses (or wearing those that belong to another)
- Mother-to-child transmission: A woman suffering from a gonorrhoeal or chlamydial infection may infect her infant during the birthing process.
Fungal conjunctivitis
Fungal infections in the body can result in either acute or chronic inflammatory reactions in the conjunctiva (the thin, transparent, mucous membrane that lines the front of the eye and inside of the eyelids). It’s not uncommon for fungi to occur in the conjunctiva but the majority do not affect conjunctival tissues too adversely. Many fungi species occur both indoors and outdoors where fungi spores can be easily inhaled. The majority of fungi that does make contact with humans rarely multiplies and thus causes very few infectious eye conditions.
Of the species that may result in rare conjunctiva infections, Aspergillus flavus (mould) tend to occur more often5.
Others include:
- Fusarium solani (a filamentous fungi)
- Candida (yeast)
- Sporothrix schenckii
- Paracoccidioides brasiliensis
- Pneumocystis jirovecii (yeast-like fungus)
Typically, fungal infections are more prevalent in climates which are warm and humid. In general, there are no specific clinical indications of fungal conjunctivitis. Many signs and symptoms can mimic other medical conditions of the eye too. These can include atypical papilloma lesions (small, wart-like growths) or conjunctival granuloma (small nodules). Individuals with weakened or compromised immune systems, such as those with HIV/AIDS, tend to experience more severe fungal infections of the conjunctiva.
Parasitic conjunctivitis
Parasitic agents are also known to cause subacute and chronic inflammation of the conjunctiva, although such infections are considered rare. Signs and symptoms relating to parasitic infections are often atypical. Skin nodules (and not just those affecting the eye) along with other symptoms like intense itching and a mucus / pus discharge are typical indications of a possible parasitic infection.
Parasitic agents which most typically cause conjunctivitis infections relate to specific habits / geographical locations. Those parasites most prevalent in one area are more likely to be the primary infection cause in that particular region over another. A doctor presented with a possible parasitic infection will need to factor in local sanitation of the area, as well as known parasite transmission modes of prevalent organisms and their often, complex life cycles.
Parasitic classes which have been associated with conjunctival infections include6:
- Protozoa (single cell organisms, such as acanthamoeba species and toxoplasma gondii)
- Nematodes (e.g. roundworms - Loa loa, toxocara canis, toxocara cati and onchocerca volvulus)
- Cestodes (e.g. tapeworms - solium cysticercus, multiceps larvae and echinococcus granulosus)
- Trematodes (e.g. flatworms, known as flukes - fasciola hepatica and schistosoma species)
- Ectoparasites (parasites that can live outside of a host, such as flies and their larvae, fleas, ticks, mites and lice)
2. Non-infectious conjunctivitis
Non-infectious conjunctivitis, as the term implies, is not caused by microscopic germs such as viruses and bacteria, but rather due to external aggravators. The types of non-infectious conjunctivitis are classified according to their various causes (which can sometimes overlap) as follows:
- Allergic
- Chemical (toxic)
- Irritants (contact lenses, foreign bodies, radiation)
- Dry Eye
- Endogenous or autoimmune
- Idiopathic
- Self-inflicted (or factitious)
- Neoplastic
Of these forms, allergic conjunctivitis and chemical conjunctivitis are the most common, as such, these will be the main focus.
Allergic conjunctivitis
Eye irritants such as dust, dust mites, mould spores, pollen and animal dander are common allergens known to cause allergic conjunctivitis (inflammation of the eye – specifically the conjunctiva and cornea). Bouts of allergic conjunctivitis may thus occur seasonally (as in the case of pollen allergies) or flare-up periodically throughout the year, when exposed to certain allergens, like pet dander or dust. Allergic conjunctivitis can also occur as a result of exposure to certain medications or the use of cosmetics, chemical scents, perfumes and fragrances or household detergents.
Following contact with an allergen, the antibody, immunoglobulin E (IgE) triggers mast cells (white blood cells) in the mucous lining of the airways and eyes. This immune system response causes the body to react to a ‘perceived threat’, and release an organic nitrogenous compound called histamine (an inflammatory substance released as part of the body’s immune response). The secretion of histamine results in the dilation of blood vessels, which then causes irritation to the nerve endings in the eye, stimulates tear production and results in allergic conjunctivitis symptoms.
An allergic cause will not result in a contagious infection and thus cannot be spread from one person to another. Those with allergy related conditions, like asthma, eczema or hay fever are typically more susceptible to experiencing allergic conjunctivitis.
Allergic conjunctivitis can also be classified by immunological reactions (or hypersensitivity reaction levels) experienced in the conjunctiva and cornea:
- Type 1 (an immediate hypersensitivity response)
- Type 2 and Type 3 (symptoms occur within a day)
- Type 4 and 5 (the onset of symptoms typically occurs after 48 hours).
Sub-types of allergic conjunctivitis include:
- Acute allergic conjunctivitis / seasonal allergic conjunctivitis / allergic rhinoconjunctivitis: This type commonly occurs seasonally, such as during seasons when pollen counts are at their highest (i.e. spring and summer). The condition normally occurs over the short-term, flaring up and resolving fairly quickly. Eyelids may begin to itch or burn as swelling occurs. A blocked or runny nose, itchy nose, and sneezing are also common with an acute allergic reaction. The combination of symptoms, along with itchy and watery eyes, with signs of conjunctivitis, is known as hay fever.
- Chronic allergic conjunctivitis / perennial conjunctivitis (all-year round): Light sensitivity, burning and itching sensations associated with a chronic case of allergic conjunctivitis can occur year-round, but this is generally less severe than an acute reaction. Triggering allergens include foodstuffs, animal dander (pets), dust and dust mites.
Sub-types of allergic conjunctivitis which occur less frequently are:
- Atopic keratoconjunctivitis (AKC): Often a result of underlying allergic types of conditions such as hay fever, atopic dermatitis, eczema and asthma. Allergens which trigger these conditions may exacerbate pink eye symptoms. Symptoms can occur at any time of the year but may present as flare-ups during specific seasons.
- Contact conjunctivitis / contact dermatoconjunctivitis: Cosmetics / make-up, shampoos and chemical products, including eye-drops can cause an allergic reaction in those with heightened sensitivities to certain substances. Conjunctivitis may develop within 2 to 4 days following contact with an aggravating substance.
- Vernal conjunctivitis (or limbal and tarsal vernal keratoconjunctivitis / VKC or spring catarhh): A long-term inflammation or swelling that affects the conjunctivae as a result of an allergic reaction is known as vernal conjunctivitis. Those with a strong family history of allergies are most susceptible to this type of allergic conjunctivitis, especially if affected by allergic rhinitis (hay fever), eczema or asthma. Triggers include irritants like pollen, cigarette smoke, chlorine (chemicals used in swimming pools) and certain ingredients in some cosmetic products.
The limbal form of the condition is characterised by a broad, thickened gelatinous and rounded opacification of the limbus (the border of the cornea and the sclera), sometimes with Horner-Trantas dots (raised, white deposits of eosinophils, disease fighting white blood cells, at the limbus)
The tarsal form is characterised by cobblestone papillae (small, rounded bumps) present on the superior tarsal conjunctiva (the upper lining of the eyelid consisting of two thick elongated plates of dense connective tissue located in each eyelid, just above the lid margins, for form and support). Each tarsus has an upper and lower portion. The smooth superior tarsal muscle connects with the levator palpebrae superioris muscle, which assists with raising the upper eyelid. - Giant papillary conjunctivitis: The use of contact lenses is particularly uncomfortable for some and can result in this type of conjunctivitis, which is also known as contact lens–induced papillary conjunctivitis (CLPC). Those with a particular sensitivity to contact lenses may find that irritation becomes progressively worse, resulting in symptoms of conjunctivitis (i.e. papillary changes in the tarsal conjunctiva). This type of conjunctivitis has also been associated with infections caused by poor hygiene when handling contact lenses, their casings and cleaning solutions. For the most part, this type of allergic conjunctivitis is caused by the chronic presence of a foreign body (like contact lenses) and can occur frequently in those who wear a prosthetic eye (ocular prosthetics) or following a surgical procedure whereby a suture (stitch) is exposed on the surface of the eye or where elevated corneal scars have developed.
Toxic /chemical conjunctivitis
Foreign substances, such as fumes, smoke, air pollution, vapours, dust or chemicals (like chlorine) can cause enough irritation to the eyes to result in chemical conjunctivitis (also known as reactive conjunctivitis).
Preservatives in eye drops (artificial tears), eye (ocular) medications, antivirals or contact lens solutions can also cause hypersensitivity, toxic and irritant reactions that are sometimes referred to as toxic conjunctivitis.
Preservative substances known to result in these kinds of reactions include:
- Benzalkonium chloride (BAK or BAC) - a common preservative ingredient in antibiotic eye drops, lubricating eyedrops and topical antiviral medications.
- Thimerosal – an antifungal or antiseptic agent.
- Stabilized oxychloro complex (SOC) – an oxidative-type preservative often used to eliminate fungi.
- Sodium perborate – a water-soluble chemical compound and oxidative preservative.
- Chlorobutanol
The use of topical medications for eyes may lead to toxic conjunctivitis within a matter of days. Sometimes reactions may occur only after extended use of topical medications. In this instance, the condition could occur following a few years of use. The severity of reactions may be dose-dependent and is often linked to the concentration of preservatives in a particular medication, or a cumulative amount if multiple products are being used. Medication-related toxic conjunctivitis is common among those undergoing chronic treatment for conditions like glaucoma – as affected people often use multiple products.
Medication-related conjunctivitis can occur as a result of:
- Neomycin (an aminoglycoside antibiotic)
- Gentamicin / Garamycin (an antibiotic)
- Idoxuridine (an anti-herpesvirus antiviral)
- Trifluoro-thymidine drops (an anti-herpesvirus antiviral)
The most common sign of exposure is conjunctival hyperaemia (red eye). Inflammation and hypersensitivity are also common indicators. Eyes that come into contact with chemicals or other offending substances can be flushed or cleaned, relieving symptoms. This form of conjunctivitis can clear up within a day or two and is not contagious.
Conjunctivitis due to irritants (contact lenses, foreign bodies, radiation)
Sleeping while wearing lenses or unhygienic handling (i.e. using tap water to rinse lenses or wearing lenses when exposed to water – showering, swimming etc.) can cause irritation and inflammation, resulting in non-infectious conjunctivitis.
Foreign substances that are applied around the eyes, such as cosmetics, can induce conjunctival inflammation. ‘Foreign bodies’ is often a term used to define the presence of substances such as grit, sand or glass which has somehow lodged in the eye. A foreign body sensation in the eyes is most often worse when an affected person blinks. This could indicate its location in the inner conjunctival surface of the upper eyelid.
Chronic conjunctivitis that is unilateral (i.e. occurs in one eye) is often suggestive of a foreign body cause. Such irritants may possibly have been retained in the fornix (the loose folds that connect the conjunctival membrane lining on the inside of the eyelid and the conjunctival membrane that covers the eyeball) or the lacrimal sac (the upper end of the nasolacrimal duct or tear duct), resulting in inflammation.
Radiation influences can occur as a complication of cancer treatment. Chemosis (swelling of the conjunctiva) can occur within days of treatment, resulting in acute conjunctivitis. If ulceration occurs, the risk of infection increases. Chronic ulceration can also occur which may result in tear film instability and dry eye.
Dry Eye
If the eyes have difficulty in maintaining an adequate coating of tears (lacrimal secretion), dry eye disease / syndrome can occur. A deficiency in tears and conjunctival mucus, as well as heat, wind or sun exposure can contribute to problems with dry eye. Foreign-body sensations, ocular irritation, blurry vision and mucoid discharge are some of the most common symptoms of the condition.
Some dry eye disorders / syndromes affecting the ocular surface include:
- Xerosis (Xerophthalmia) – a condition wherein the eyes are unable to produce tears.
- Keratoconjunctivitis sicca (associated with Sjögren syndrome) – also known as dry eye disease or dry eye syndrome, resulting in tear film instability, visual disturbance and ocular surface discomfort.
- Symblepharon – a condition wherein an adhesion, either partially or completely, forms between the palpebral conjunctiva (i.e. the clear membrane on the inside lining of the eyelids) and bulbar conjunctiva (i.e. the clear membrane which covers the outer surface of the eyeball).
- Conjunctivochalasis – a condition characterised by excess folds on the conjunctiva, usually in between the margin of the eyelid and the eyeball.
- Argyrosis (ocular) – a condition characterised by ocular discolouration following local or systemic absorption and chronic exposure to silver.
Endogenous or autoimmune conjunctivitis
Autoimmune diseases that are known to affect the mucous membranes of the body can contribute to underlying non-infectious conjunctivitis symptoms (with these ranging from mild to severe). Conjunctival redness and discharge may be present in several types of systemic medical conditions7.
Some of these include:
- Primary Sjögren syndrome (an immune condition characterised by dryness of the eyes and mouth without the presence of another autoimmune condition)
- Kawasaki disease (a rare condition affecting the body’s blood vessels and mucous membranes)
- Carotid cavernous fistula (abnormalities involving the carotid arterial system and the cavernous sinus)
- Stevens-Johnson syndrome (a rare condition involving the mucous membranes of the body, as well as the skin – ulcerative lesions can occur in the eyes)
- Mucous membrane pemphigoid (a rare group of autoimmune conditions characterised by blistering lesions affecting the eyes and mouth - Ocular cicatricial pemphigoid is a subtype of this group of conditions that results in autoimmune conjunctivitis)
- Reiter disease (a type of reactive arthritis / systemic rheumatic condition which can result in eye inflammation)
- Behçet's disease (a rare multisystem condition involving inflammation of the eyes)
- Sarcoidosis (another multisystem condition resulting in inflammation of the eyes, and various other portions of the body, including the skin and the lungs)
Idiopathic conjunctivitis
Conjunctivitis that is considered idiopathic typically means that a condition spontaneously arises, and an underlying cause cannot be distinctively determined. It is, however, relatively rare for an underlying cause of conjunctivitis not to be identified.
Some instances where conjunctival issues occur due to an unknow cause include:
- Ligneous conjunctivitis - A rare and chronic condition that is common among children, particularly girls. An accumulation of fibrin (protein) results in conjunctival inflammation and the formation of thick, woody growths which are often white, yellow or red in colour8.
- Subconjunctival haemorrhage – A benign eye condition that is generally considered idiopathic as in the majority of cases an underlying cause is unknown9. The condition is characterised by redness (bleeding) beneath the conjunctiva and inflammation. Bleeding may be dot or blotch-like or more extensive, rendering the sclera (white outer layer of the eyeball) difficult to see.
Self-inflicted (or factitious) conjunctivitis
Conjunctival inflammation can also be as a result of self-inflicted harm. Such harm can be physical in nature (i.e. deliberately causing conjunctival or corneal lacerations and abrasions) or chemical. A person may make use of medications too, purposefully exposing them to the eye. Self-inflicted conjunctivitis instances are referred to as factitious keratoconjunctivitis10.
Self-inflicted conjunctivitis is sometimes associated with psychiatric problems or diseases. It has been noted in paediatric syndromes linked with severe mental retardation, schizophrenia or even heavy illicit drug use. In the case of psychiatric self-inflicted harm, injury to the eye is typically as a result of direct blows to the head (i.e. headbanging) or intentional lacerations11.
A doctor may suspect self-inflicted harm should it be determined that a patient has inexplicably poor surface healing of the eye (conjunctiva) or if he/she displays a recurrent breakdown of the thin tissues on the outer layer of the cornea.
Neoplastic conjunctivitis
Neoplasms (i.e. abnormal tissue growth on the surface of the eye) can occur as either benign or malignant tumours, which result in conjunctival inflammation. In many instances, these tumours originate in the conjunctiva (or inside of the eyelid lining) and can result in cancerous eye conditions like squamous carcinoma, lymphoma and malignant melanoma.
Conjunctivitis in new-born babies (Neonatal conjunctivitis / ophthalmia neonatorum
All instances of pink eye in infants and young babies (which normally present within the first 2 weeks of life) should be evaluated by a medical professional immediately12.
Underlying causes can be as a result of an infection, especially those transmitted from a mother during childbirth such as herpes, gonorrhoea or chlamydia; a blocked tear duct (caused by irritation from the application of topical antimicrobials, usually a silver nitrate solution, given shortly after birth to prevent infection); or exposure to a particular kind of irritant (such as a chemical – this is known as aseptic neonatal conjunctivitis). In most instances, symptoms will normally resolve within 24 to 36 hours.
Neonatal conjunctivitis caused by an infection (viral or bacterial – referred to as septic neonatal conjunctivitis), in particular, must be medically evaluated as soon as possible, so as to reduce the risk of potentially severe complications or permanent damage in a young baby.
It is common for new born babies to develop an eye discharge without redness. Interestingly, this can easily be treated by putting the mothers breastmilk in the eye.
Who is most at risk of developing conjunctivitis / pink eye?
- The risk of developing conjunctivitis increases for anyone who is exposed to the viral or bacterial causes of conjunctivitis, this is especially elevated in those who work in or attend community-type environments such as schools, hospitals, prisons, old age homes and care facilities.
- Those who are prone to allergies tend to develop allergic conjunctivitis more frequently, especially if contact is made with triggering allergens.
- Those who use extended-wear contact lenses.
References:
2. Review of Ophthamology. 19 March 2010. A guide to understanding adenovirus, the diseases it causes and the best ways to treat these conditions: https://www.reviewofophthalmology.com/article/a-guide-to-understanding-adenovirus-the-diseases-it-causes-and-the-best-ways-to-treat-these-conditions [Accessed 14.02.2018]
3. Pathology of the Eye. 1980. Conjunctiva: https://books.google.co.za/books?id=yI_TBwAAQBAJ&pg=PA262&dq#v=onepage&q&f=false [Accessed 14.02.2018]
4. Ophthamology (Fourth Edition). 2009. Part 4: Cornea and Ocular Surface Diseases - Conjunctivitis: Infectious and Noninfectious: https://books.google.co.za/books?id=nTvRAQAAQBAJ&pg=PA183&dq#v=onepage&q&f=false [Accessed 14.02.2018]
5. Blepharitis and Conjunctivitis: Guidelines for Diagnosis and Treatment. 2006. Infectious Conjunctivitis: https://books.google.co.za/books?id=J3tqqfA6EC4C&pg=PA104&lpg=PA104&dq#v=onepage&q&f=false [Accessed 14.02.2018]
6. InTech Open. 9 May 2016. Ocular Parasitic Infections – An Overview: https://www.intechopen.com/books/advances-in-common-eye-infections/ocular-parasitic-infections-an-overview [Accessed 14.02.2018]
7. Parsons' Diseases of the Eye (22nd Edition). 2015. Chapter 14 - Diseases of the Conjunctiva: https://books.google.co.za/books?id=JTJTBwAAQBAJ&pg=PA167&dq#v=onepage&q&f=false [Accessed 14.02.2018]
8. Oxford Handbook of Ophthamology (Third Edition). 2014. Chapter 6 -Conjunctiva: https://books.google.co.za/books?id=jtqSBQAAQBAJ&pg=PA206&dq#v=onepage&q&f=false [Accessed 14.02.2018]
9. US National Library of Medicine - National Institutes of Health. 12 June 2013. Subconjunctival hemorrhage: risk factors and potential indicators: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702240/ [Accessed 14.02.2018]
10. Training in Ophthamology - The Essential Clinical Curriculum (Second Edition). 2016. Conjunctivitis IV - Miscellaneous: https://books.google.co.za/books?id=ila1DAAAQBAJ&pg=PA60&dq#v=onepage&q&f=false [Accessed 14.02.2018]
11. Pediatric Ophthalmology and Strabismus. 2013. Self-inflicted conjunctivitis: https://books.google.co.za/books?id=bDygdHfaqTcC&pg=PA1067&dq#v=onepage&q&f=false [Accessed 14.02.2018]
12. Centers for Disease Control and Prevention. 2 October 2017. Conjunctivitis (Pink Eye) in Newborns: https://www.cdc.gov/conjunctivitis/newborns.html [Accessed 14.02.2018]

