- Gum Disease (Gingivitis)
- What is the difference between gingivitis and periodontitis?
- What are the symptoms of gingivitis?
- What causes gingivitis?
- What are the risk factors and complications of gingivitis?
- How is gingivitis diagnosed and treated?
- Can gingivitis be prevented?
- How to practice good oral hygiene
- Some more information on gum disease
What is the difference between gingivitis and periodontitis?
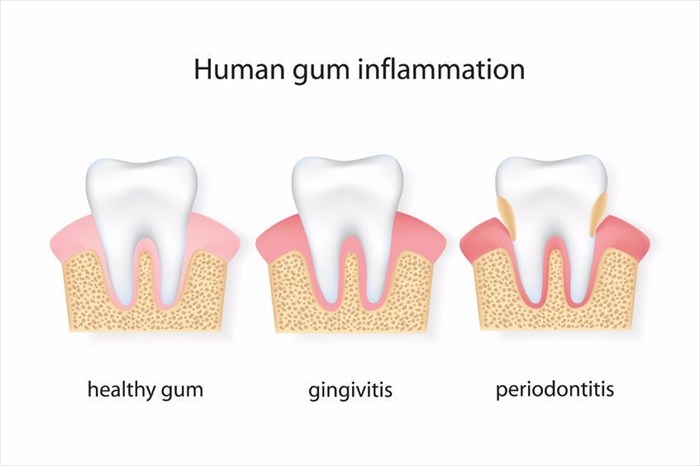
Gingivitis that is left untreated can progress and develop into periodontitis, a condition that may lead to tooth loss as well as a number of other complications and health problems. The below explanation gives a brief outline on the difference between the two conditions:
Gingivitis
This is the mildest form of gum disease, also known as periodontal disease, wherein the gums will become swollen, red and may bleed easily. At this stage, there is typically very little discomfort. Gingivitis can be reversed through professional dental care and personal oral hygiene.
The factors that may have a role to play in the development of gingivitis can include:
- Puberty
- Aging
- Smoking
- Inadequate nutrition
- Pregnancy
- Genetic predispositions Diabetes
- Stress
- Hormonal changes
- HIV infection
- Certain medications
- Systemic diseases
Periodontitis
When gingivitis is left untreated, it can advance and develop into periodontitis. In time, the plaque (this is a sticky deposit/fill that covers your teeth and contains bacteria), may grow and spread below your gum line. The bacteria produces toxins that irritate your gums and creates an inflammatory response where your body basically attacks itself and the bone and tissues that support your teeth are targeted and destroyed by the immune system.
The gums will separate from your teeth and form pockets that are infected with the bacteria. When the condition progresses, these pockets will deepen and more bone and gum tissue will be destroyed. There are a number of different forms of periodontitis, each one having different symptoms and describing a different rate at which the condition progresses.
These forms include:
- Aggressive periodontitis – This involves the rapid loss of bone and detachment of teeth.
- Chronic periodontitis – This progression of bone and gum loss is normally slower with this form of the condition and is the most commonly seen form of periodontitis. This form is characterised by the formation of pockets in the gingiva.
- Periodontitis as a result of a systemic disease – This normally starts when the patient is young and can be linked to a number of systemic diseases including cancer, atherosclerotic cardiovascular disease, diabetes, rheumatoid arthritis, chronic kidney disease, respiratory disease, metabolic syndrome and obesity, amongst others.
- Necrotizing (flesh-eating) periodontal disease – This infection is characterised by the destruction of the gum tissues, bone and periodontal ligaments. These lesions tend to appear in those who have suppressed immune systems from conditions such as HIV and malnutrition.