The general characteristic symptoms of hemorrhoids are:
- Pain, soreness or discomfort (especially during a bowel movement and around the anal area)
- Itching and irritation around the anus
- Anal swelling
- Painless bleeding (bright red in colour which indicates fresh bleeding) during a bowel movement (noticed either in a toilet bowl or after using toilet tissue paper)
- A moist lump formation near the anus (this may be extremely sensitive or painful)
- Faecal / stool leakage
- Frequent haemorrhoid developments can result in anaemia due to chronic blood loss (although this is very rare)
Symptoms specific to haemorrhoid types
Internal haemorrhoids
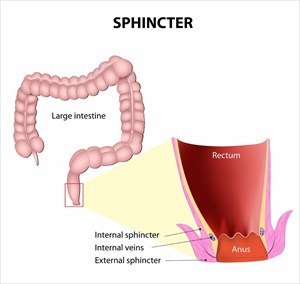
These types occur on the inside of the rectum (above the pectinate line) and are not normally seen or felt. It is also very rare for these types of haemorrhoids to cause a great deal of pain or discomfort as there are fewer pain-sensing nerves in their location of development above the pectinate line.
Bleeding, however, is an indication of their presence. Straining during a bowel movement (especially when passing a hard stool) places added pressure on veins, scraping the thin lining, resulting in swelling when the stool is passed. This causes irritation and ruptures the tissue surface leading to bleeding (without pain).
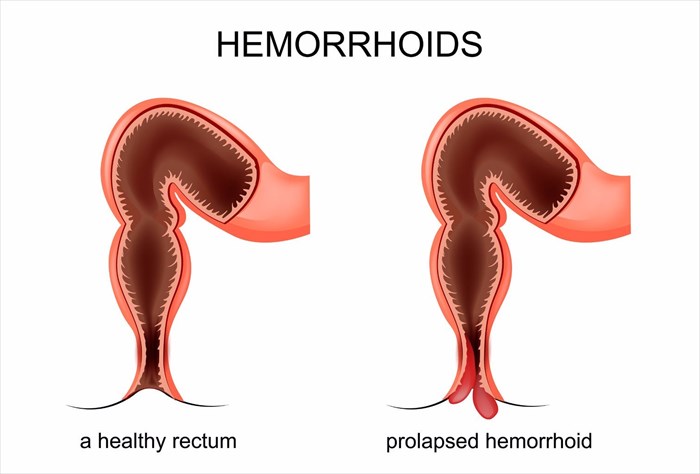
A swollen internal haemorrhoid can also result in muscle spasms around the anus and rectum. This can sometime cause pain. Straining during a bowel movement can then push internal hemorrhoids out through the anal opening (or anal sphincter). These are then referred to as protruding or prolapsed haemorrhoids and can be very uncomfortable or painful to experience due to itching and burning sensations (pruritic ani). These protruding lumps can sometimes leak mucus or collect microscopic stool particles, which can cause further symptomatic irritation.
Internal hemorrhoids are graded in relation to the degree of prolapse which occurs:
- First-degree: During a bowel movement, a haemorrhoid bulges into the anal canal (remaining inside).
- Second-degree: In this instance, during a bowel movement, the haemorrhoid bulges further (from the anus) and then retracts (goes back inside the anal canal).
- Third-degree: This degree of prolapse is similar to a second-degree, but the haemorrhoid bulges a little further out of the anus and does not easily retract on its own. The hemorrhoid can be returned inside by physically pushing it back (i.e. with a finger).
- Fourth-degree: These haemorrhoids prolapse out of the anus and remain on the outside of the body (i.e. do not go back on their own).
External haemorrhoids
External hemorrhoids can result in the development of excess skin tags (short and narrow skin growths) near the anal verge (anal opening / anus). These can often make for difficult cleaning after a bowel movement, and sometimes lead to secondary skin infections. Consistent straining, cleaning and rubbing around the anus can worsen haemorrhoid symptoms. It’s fairly common for symptoms of external haemorrhoids to resolve within a few days.
If blood pools within an external haemorrhoid, forming a thrombus (clot), a thrombosed haemorrhoid develops (these can also develop from internal haemorrhoid types). This can result in severe pain and discomfort, inflammation, swelling and the development of a hard and painful lump which develops a purplish-blue discolouration near the anal opening. The pain associated with these types of hemorrhoids usually peaks on the second or third day and begins to resolve from the fourth day onwards as the clot is reabsorbed by the body. Even though a thrombus dissolves, it may leave behind a little skin, which can still be subjected to irritation.
How long do the symptoms of haemorrhoids last?
Small external haemorrhoids typically only really present symptoms over a few days (without treatment). A prolapsed haemorrhoid can take longer to heal, requiring medical treatment. A woman who develops hemorrhoids during pregnancy may experience symptoms until she has delivered her baby (given birth), after which they usually spontaneously resolve, especially if constipation is actively prevented.
When to call the doctor if you have haemorrhoids
The presence of blood, whether accompanied by pain and discomfort or not is not normal, and should never be disregarded. Bleeding from the rectum / anus may be as a result of a relatively benign cause, such as a haemorrhoid, but a medical doctor will need to conduct a thorough medical assessment in order to determine this.
Rectal bleeding and or/ the presence of blood in stool (faeces) can sometimes signal a more serious cause, which can be life-threatening. Potentially more severe reasons can include inflammatory bowel disease (such as ulcerative colitis or Crohn’s disease), a bleeding ulcer, colon polyps, anal fissures, diverticulitis or tumours (cancer of the rectum or colon).
Other than bleeding, a marked change in bowel movements, such as a change in consistency or colour of stools, must also be evaluated by a medical doctor. Tests may rule out various conditions, but can also help to determine possible signs of extensive bleeding which may be taking place elsewhere in the digestive tract.
Pain (which persists longer than a few days to a week) or a lack of improvement for existing haemorrhoids (within a two-week period) should also be looked at by a medical doctor. Large quantities of blood loss (or an increase in rectal bleeding quantity), dizziness, light-headedness or fainting must be attended to by emergency medical professionals immediately.
While the thought of consulting a doctor regarding any type of issue related to the anus may seem a little mortifying, this is a natural but unwarranted response as most medical professionals have conducted countless anal examinations during the course of their careers. As such, there is no need for embarrassment.
An anal examination is neither the most comfortable or pleasant experience for the person concerned, but is generally quick and painless, causing only slight discomfort. It can also help a doctor to make an accurate diagnosis and advise on the most effective methods of treatment to rapidly resolve any discomfort being experienced. Most importantly, it may even save one’s life as the more sinister diseases such as anal or colon cancer have a higher treatment success rate when detected early.