Risk factors and complications associated with hepatitis
What are the main risk factors for hepatitis?
- Hepatitis A: If you travel to or live in areas with high infection rates, have unprotected sex with multiple partners, work in child care centres or nurseries and handle children, are HIV positive, use injected drug substances (intravenously i.e. injected into your vein), have a clotting-factor disorder (such as haemophilia), or have direct contact with an infected individual (that you live with).
- Hepatitis B: You may be high risk if you have multiple sex partners (with whom you have unprotected sex), are a healthcare worker, use IV drug substances, have a chronic liver disease or kidney disease, or if you travel or live in high infection rate areas.
- Hepatitis C: Risk is higher if you received a blood transfusion or had an organ transplant before 1992, were born to an infected mother, have had unprotected sex with an infected person, shared contaminated needles (when using illicit drugs, having body piercings or tattoos), are a healthcare worker exposed to infected blood, have HIV, received clotting factor concentrates before 1987, received haemodialysis (for an extensive period of time) or were ever imprisoned (this increases the risk of infection due to the sharing of personal care items between inmates).
- Hepatitis D: You may be at increased risk if you have an HBV infection already, often receive blood transfusions, have unprotected sex or use IV drug substances.
- Hepatitis E: Risk is higher in areas with frequent water contamination (especially resource – limited / developing countries or those affected by war, refugee camps and internally displaced populations).
- Alcoholic hepatitis: Heavy drinking (or binge drinking), weight (obesity), a person’s sex (females have a higher risk due to the way alcohol is processed in the body), some genetic and environmental factors and race or ethnicity (African-Americans and Hispanic people are higher risk).
- Autoimmune hepatitis: If you have a history of infections with measles, herpes (herpes simplex virus 1 and 2) or Epstein-Barr virus, if you are female (occurrence rates are higher in females than males), if you have a predisposition to autoimmune hepatitis (may run in families), have an autoimmune disease (such as celiac disease, hyperthyroidism or rheumatoid arthritis).
What types of complications are common with hepatitis infections?
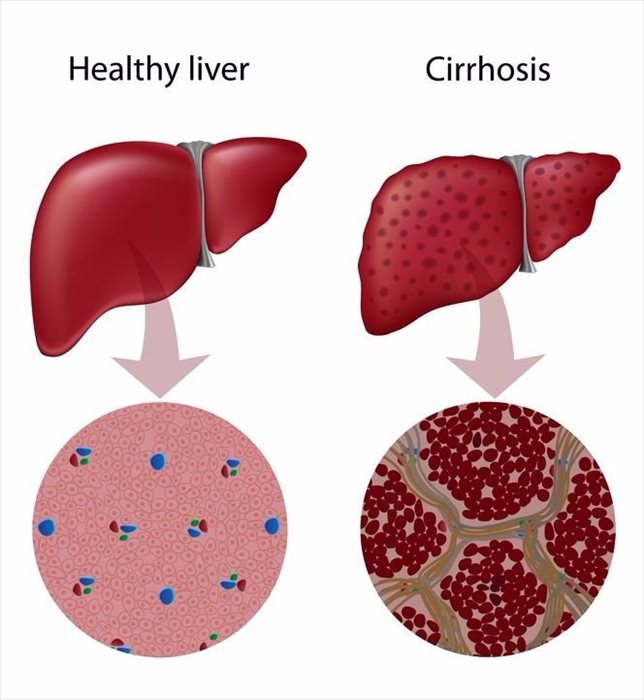
Acute hepatitis generally doesn’t lead to any long-term concerns. Chronic HBV and HCV commonly lead to more serious complications if damage is caused to the liver. Complications can include cirrhosis, acute and chronic liver disease, and cancer of the liver.
Liver failure is another complication which results in a build-up of fluid in the abdomen, bleeding disorders, kidney failure, increased blood pressure in the liver’s portal veins, hepatic encephalopathy and hepatocellular carcinoma (a form of liver cancer). If this happens you will be hospitalised and monitored very carefully.
A viral infection that isn’t well managed can lead to further damage to the liver and total failure. A medical professional will strongly advise you to avoid alcohol consumption, certain supplements and specific prescription and over-the-counter medications that will have an adverse effect on the liver.
Complications for alcoholic and autoimmune hepatitis can include varices (enlarged veins restricting blood flow and causing bleeding), high blood pressure in the liver (restricted blood-flow can lead to scarring and increased pressure in the portal vein), ascites, jaundice, hepatic encephalopathy, cirrhosis and kidney failure. Autoimmune hepatitis can also result in liver failure and liver cancer.