Understanding sleep and wakefulness
It is believed that quality sleep achieved at the correct time every day is as important for human survival as food and water consumption. As a biological need, sleep is an important factor for daily function. It affects virtually all bodily systems and tissues, and if enjoyed in sufficient quantities and quality, adds to a person’s overall health. When severely lacking, the influence falls to the other end of the scale and can place a person at risk of developing a variety of health issues including blood pressure problems and mood disorders like depression.
While necessary, sleep functions in a very complex and dynamic way, influencing both the brain and body which remain active throughout. Some of this is fairly well understood in clinical circles, while various aspects are still being comprehensively researched. So, in terms of what is known, what actually happens when we sleep?
Stages of sleep
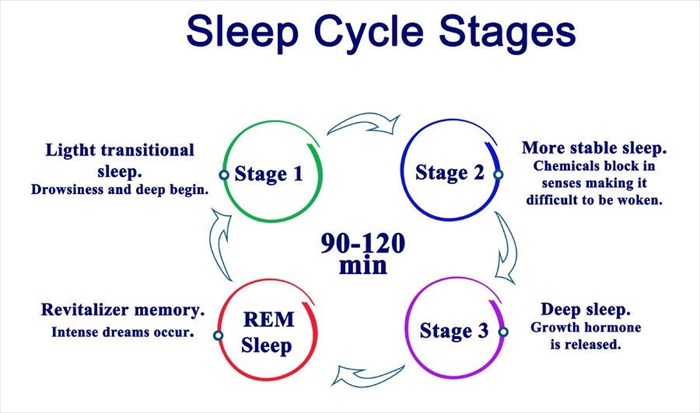
There are two primary stages of sleep – non-REM (non-rapid eye movement) sleep and REM (rapid eye movement) sleep.
Each stage or phase of sleep is associated with various brain wave and neuronal activity. A person generally shifts through all stages and phases of sleep in cycles during the night. Longer and deeper REM phases typically occur during the early hours of the morning.
1. Non-REM sleep
This phase of sleep can be sub-divided into three stages:
- Stage 1: This stage of non-REM sleep is a short changeover from wakefulness to light sleep, which generally lasts a few minutes. A person’s heartbeat, eye movements and breathing begin to slow down, and the body’s muscles relax, often with occasional twitch movements. Brain wave patterns also begin to slow down, becoming less active than they are during wakefulness.
- Stage 2: This is the stage of light sleep before falling into a deep sleep state. Breathing slows down a little more, as does a person’s heartbeat. Eye movements cease and body temperature decreases. Occasional bursts of electrical activity (i.e. brain wave activity) take place, but these are generally brief. A person typically spends more of their sleep cycles in this sleep stage than any other.
- Stage 3: This is the stage of deep sleep which is necessary for the body to feel refreshed the next day. The initial cycles of this stage are generally longer during the first half of the sleep period. A person’s heartbeat and breathing are at their slowest. Brain wave activity slows even further, and the body’s muscles are completely relaxed, so much so it may be difficult to awaken a person from their sleep.
2. REM sleep
REM sleep generally occurs approximately 90 minutes after falling asleep. (3) During this time, the eyes move from side to side in a rapid motion behind a person’s closed eyelids. Breathing quickens and becomes more irregular, and a person’s blood pressure and heart rate also increase. Mixed frequency brain wave activity during this stage is similar to that which occurs while a person is awake.
It is during REM sleep that dreaming most typically occurs although it is possible to experience a little dreaming during non-REM sleep too. While dreaming, muscles in the arms and legs become temporarily paralysed. This form of paralysis is referred to as REM atonia, a phenomenon wherein the brain temporarily suspends the stimulation of the large muscle groups in order to prevent a person from being physically able to act out or move during a dream sleep state.
Brain structures and sleep
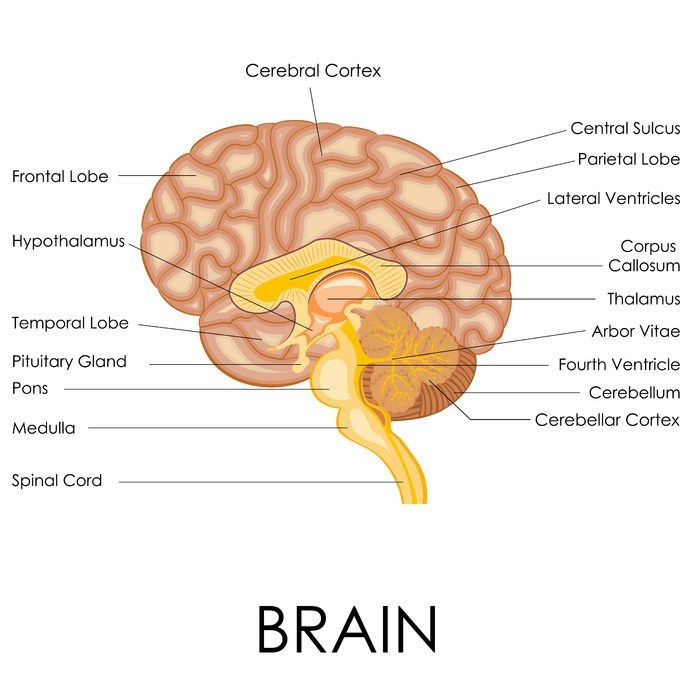
Brain structures that are involved in the sleep process are:
- The hypothalamus: This tiny structure located deep inside the brain consists of numerous groups of nerve cells which help regulate sleep and wakefulness. This structure also contains groupings of thousands of cells (i.e. the suprachiasmatic nuclei / SCN) which receive light exposure information from the eyes. This helps to manage behavioural rhythm. If there is any damage to this nucleus, impairments to a person’s circadian rhythms occur.
Did you know? Many blind individuals do have some sense of light, which means that the hypothalamus and SCN can still naturally moderate their sleep/wake cycles to some extent. Those who do not have any sense of light can better promote sleep/wake cycles by taking regular synthetic dosages of the hormone, melatonin at the same time every day to assist the body in coordinating sleep patterns with the times when sleep should be achieved.
- The brain stem: At the base of the brain, the pons, medulla and midbrain structures ‘communicate’ with the hypothalamus and thereby help to moderate the transitions between wakefulness and sleep. Together with the sleep promoting cells of the hypothalamus, the brain neurotransmitter, GABA (Gamma-aminobutyric acid) is produced, which processes chemical messages through the brain and the nervous system. GABA reduces the activity of the hypothalamus and brain stem’s arousal regions, sending signals to muscles to relax. Relaxation settles the posture of the body and prevents limb movements during a dream state.
- The thalamus: Located just above the brain stem, and between the mid brain and cerebral cortex, the thalamus has a vast number of nerve connections which serve as transmitters for information. Relayed information stems from the body’s senses to the cerebral cortex, which serves as the covering of the brain. Here information is processed from short-term to long-term memory. The thalamus is a small structure which becomes quiet during most stages of sleep. This is what effectively allows a person to ‘zone out’ from the external world. During REM sleep, however, the thalamus remains active, continuing to process cortical images, sensations and even sounds – these are believed to ‘feed’ a person’s dreams.
- The pineal gland: Situated between the brain’s two hemispheres, the pineal gland receives signal messages from the suprachiasmatic nucleus (SCN). This prompts the increased production of melatonin, which helps to promote a state of sleep. As a natural hormone, its production and release correspond with the time of day, peaking in the evening (to encourage sleep) and reducing during the morning (to promote wakefulness). If a person is exposed to light at night when production and secretion activity is at its highest, this can block the process / circadian rhythm, and thereby disrupt sleep.
- The basal forebrain: Situated near the front and bottom portion of the brain, the basal forebrain secretes the chemical adenosine, which is a by-product of cellular energy consumption. Neuronal discharge (i.e. cholinergic neurons) during periods of wakefulness result in increased metabolic activity and an accumulation of adenosine. During the day this is important for cognitive function. The secretion of accumulated adenosine helps to support a sleep state by inhibiting the neurons responsible for wakefulness and allowing sleep-related neurons to become active. If a person consumes caffeine too close to a routine bedtime, the actions of this ‘sleepy’ chemical are counteracted, thus preventing sleep or causing disruptions to it.
- The amygdala: Almond-shaped structures, two amygdalae exist on either side of the brain. Each amygdala forms part of the limbic system, which is responsible for processing and regulating emotions, behaviour, survival instincts, motivation, and the formation of emotional memories. These structures are selectively activated during REM sleep and it has been suggested that they may be responsible for the emotional content of dreaming during an REM sleep cycle. The amygdala is also associated with the reprocessing and strengthening of emotional experiences while engaged in REM sleep.
Mechanisms of sleep
There are two main biological mechanisms associated with sleep – circadian rhythms and homeostasis. These mechanisms work together in order to help regulate both sleep and wakeful states.
- Circadian rhythms: These rhythmic processes help to regulate the timing of sleep, when a person begins to feel sleepy, as well as when the ‘internal body clock’ arouses a person from a sleep state (without a mechanism like an alarm to force wakefulness). Circadian rhythms are thus involved in the daily fluctuations of body temperature, hormone secretion and metabolism which influence these states during a 24-hour period.
- Homeostasis: Originating from the Greek word meaning “steady” or “the same”, homeostasis refers to a process which actively maintains the stable conditions necessary for survival (i.e. equilibrium) within a living organism regardless of changes in its environment. In this way, bodily functions can be better balanced.
Sleep-wake homeostasis helps to keep track of the need for sleep, ‘reminding’ the body that sleep is necessary. It also helps to regulate the intensity of sleep. The drive for sleep strengthens each hour that a person is awake and promotes longer periods of sleep once it is initiated.
Disruptions to this sleep-wake mechanism interfere with its function. These can include the likes of medical conditions, stress, medication use, the consumption of certain foods and beverages, as well as changes in one’s sleep environment. Light exposure, in particular, can disrupt the function of this mechanism by delaying the process of sleep. It can also disrupt the initiation of sleep or returning to sleep if one wakes up during the night or early morning hours.
How much sleep do we really need?
It’s challenging to pinpoint an actual number of hours of sleep required as sleeping patterns typically change as human beings age and can even vary among individuals of the same age. Thus, there is no ‘magic number’ that is applicable to everyone, but rather an average range pertaining to the different life stages of a person. (4)
- An infant (0-3 months old) will initially require between 14 and 17 hours of sleep in a 24-hour period. This is necessary in order to help promote growth and development, particularly of the brain.
- After 3 months a baby will normally require between 12 and 15 hours per day.
- Toddlers between the age of 1 and 2 require between 11 and 14 hours of sleep within a 24-hour period.
- Pre-schoolers (aged 3 to 5) will need between 10 and 13 hours.
- Children 6 to 13 years of age require between 9 and 11 hours of sleep.
- Once into the teenage years (14 to 17 years of age), between 8 and 10 hours of sleep a night is quite normal.
- The average adult (aged between 18 and 64) can comfortably function on between 7 and 9 hours of sleep a night.
- Sleep patterns in adults tend to adjust after the age of 60 to 65, where sleep length becomes a little shorter and lighter (7 to 8 hours), occasionally interrupted by awakenings during the night. Seniors are also more prone to taking medications for various health ailments, both of which can interfere with comfortable sleep and cause disruptions.
With plenty of distractions cutting into normal sleep routines, it can be difficult to “make up” for lost sleep. Round-the-clock entertainment and extended working hours are an acceptable norm these days, and many feel as though they can sacrifice sleep and then ‘catch up’ on it during days that have fewer lengthy commitments, like weekends.
Whether or not ‘catching up’ is sufficient enough will depend on how sleep deprived a person actually is. For a person with insomnia, ‘catching up’ will not correct the problem, but rather worsen it.
References:
3. National Institutes of Neurological Disorders and Stroke. July 2018. Brain Basics - Understanding Sleep: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep [Accessed 04.08.2018]
4. Eunice Kennedy Shriver National Institute of Child Health and Human Development. January 2016. How much sleep do I need?: https://www.nichd.nih.gov/health/topics/sleep/conditioninfo/how-much [Accessed 04.08.2018]