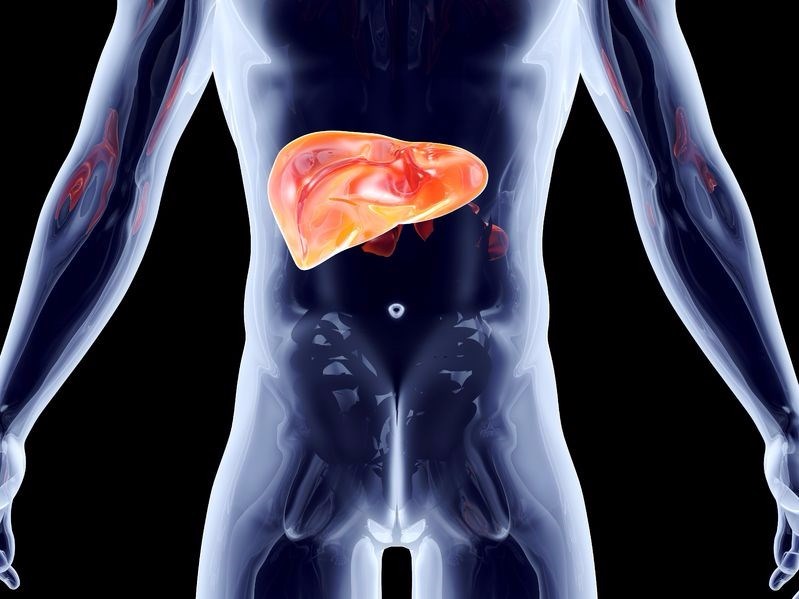
- Liver Disease / Hepatic Disease
- What are the causes/types of liver disease?
- What are the stages of liver disease from initial inflammation to liver failure?
- What are the symptoms and risk factors of liver disease?
- What is the diagnosis, treatment and prevention of liver disease?
- The liver disease diet and outlook
What are the stages of liver disease from initial inflammation to liver failure?
To put everything into perspective, it would help to explain the difference between liver disease and liver failure. Liver disease refers to the initial inflammation of the liver that can sometimes be repaired naturally by the liver itself or through effective medical treatment.
Liver disease that does not heal or is not treated can lead to liver failure when the liver is unable to perform its normal functions. Simply put, liver failure is the end-stage of liver disease and requires immediate treatment. If any functioning parts of the liver cannot be saved, then often the only alternative is a liver transplant which can be a long and complicated process of organ transplant waiting lists, evaluations and hospital visits.
The damage done to the liver and the stages of liver disease remain consistent if the condition is not treated or does not heal initially. This consistency remains the same regardless of the cause or type of the liver disease.
These stages are described as follows:
Stage One - The first stages of liver disorder/disease
The first stage of liver disease involves inflammation of the individual’s bile duct or liver. Abdominal pain is often the first symptoms of this inflammation as the person’s body attempts to fight off the disease or infection. If this inflammation is left untreated, it can result in the liver being damaged, thus worsening the condition. During stage one, the symptoms and inflammation are often treatable and can prevent liver disease from progressing to stage two.
Stage Two: Inflammation leads to scarring (fibrosis) of the liver
In a number of people with liver disease, the condition only becomes evident at stage two or during stage three as the initial symptoms often go unnoticed. Stage two consists of the scarring or inflammation (damage) starting to block the natural flow of blood in the liver. This results in the liver not being able to function correctly, however, through treatment, the liver may still be capable of healing, thus preventing any further damage from being done and halting the progression of the liver disease.
Stage Three: Cirrhosis
Cirrhosis, pronounced “si-roh-sis”, is a result of liver disease progression, usually due to lack of treatment, wherein the scar tissue of the liver replaces healthy tissue. This process occurs when the healthy liver cells have been damaged over time (normally a number of years) from a progressive disease or infection. This results in the permanent scarring of the liver making it hard and lumpy. Eventually the liver will not be able to function as the new scar tissue will make is difficult for blood to pass through the portal vein and into the liver. When this blood is blocked from entering the portal vein, it can flow into the spleen which can result in further issues.
At this stage of liver disease, damage is irreversible and a doctor will tend to focus on treatment that will protect any existing functional liver tissue and manage the symptoms so as to slow down the progression of the condition and possibly prevent the disease from advancing to complete liver failure. Cirrhosis does not have a cure and in severe cases, the patient will require a new liver entirely.
Cirrhosis stages
Cirrhosis has two key phases, these are:
- Compensated – This phase does not cause any symptoms as the healthy liver cells are still able to meet the needs of the body and compensate for the scarred tissue and damaged cells. Treatment is required at this stage in order to stop the condition from progressing to liver failure as the body will be unable to rid itself of toxins effectively.
- Decompensated – This kind of cirrhosis does cause a number of symptom and may lead to issues including:
- Bleeding of varices – Varices are blood vessels that are dilated in the stomach or oesophagus and are a result of portal hypertension from the portal vein to the liver being blocked. The increase in pressure of the liver’s portal vein results in the blood moving to other, smaller blood vessels, which are unable to hold the increased volume of blood and can rupture putting the patient at risk of a blood infection. Variceal bleeding is considered a medical emergency and requires immediate attention and treatment.
- Hepatic encephalopathy – Pronounced “en-sef-uh-lop-uh-thee”, this is the loss of functioning in the brain due to the liver being unable to remove the toxins from the patient’s blood. The symptoms are often confusion and forgetfulness.
- Ascites – Pronounced “ah-SIGH-tees”, this condition refers to the build-up of fluids, specifically the fluid containing protein known as ascetic, in the abdominal cavity (peritoneum) due to an increase in blood pressure of the blood vessels in the liver forcing fluid to accumulate in the belly.
- Jaundice – This is a condition that refers to the yellowing of the eyes and skin as a result of the elevated levels of yellow pigment existing in the body known as bilirubin. It is the responsibility of the liver to produce and process this bile pigment, if the liver and bile ducts are not functioning correctly due to scarring and damage done, this pigment accumulates.
- Gallstones – The gallbladder is found right under the liver. Gallstones are hard digestive fluid deposits and often result in the gallbladder needing to be removed if the patient suffers from the symptoms. Cirrhosis can lead to the bilirubin chemical accumulating (this is needed to break down the red blood cells) which is a contributing factor to the formation of gallstones.
Stage Four: Liver failure / advanced liver disease / hepatic failure
During the disease’s final stage, the failure of the liver will signal the termination of the functioning of the liver. This will require immediate medical attention in order to prevent fatality. The symptoms associated with liver failure may include:
- Diarrhoea
- Vomiting
- Fatigue
- Stage three symptoms
- Jaundice
- Weakness
- Itching
- Loss of appetite
- Bruising easily due to the decrease of the blood clotting components being produced by the damaged liver
It can take a number of years for cirrhosis to progress to liver failure, however the damage that has been done at this stage is irreversible and fatal.
The goal is for liver disease to be diagnosed and treated as early as possible in order for the prognosis to be improved and liver failure to be prevented.
Acute (sudden) liver failure
This type of rare liver failure rapidly progresses and liver failure occurs within a number of days or weeks. Acute liver failure tends to affect those who do not have any existing liver disease. The condition often occurs suddenly without symptoms or warning. The causes typically include drug overdose from ingesting a high amount of Tylenol (acetaminophen/paracetamol).
Chronic (gradual) liver failure
The more gradual type of liver failure is known as chronic liver failure as it can occur over a number of months or years (usually over a period of six months or more) before any symptoms are shown. This condition is normally the end result of severe liver damage/disease known as cirrhosis.
If you are concerned about your liver condition, or you have been experiencing some of the symptoms mentioned above, visit www.fibronostics.com to learn more about the available liver test option for accurate diagnosis.

