- Parkinson’s disease
- What has research for Parkinson's been able to determine?
- How does Parkinson’s disease affect the body?
- What are the stages of Parkinson’s disease?
- What factors may increase risk of Parkinson’s disease?
- Common complications and side-effects of Parkinson’s disease
- Diagnosing Parkinson’s disease
- Treating Parkinson's disease
- Living with Parkinson’s disease
- Parkinson's disease FAQs
How does Parkinson’s disease affect the body?
Recognising the signs
A combination of signs can help a doctor make an early diagnosis. If Parkinson’s disease is diagnosed early, the chances of being able to treat and manage the condition are greater. Individual signs may not be an indication of Parkinson’s disease. Some signs such as loss of smell could be caused by an infectious illness, or joint stiffness by conditions like arthritis.
Parkinson’s is most commonly diagnosed with a very physical examination and assessment of a person’s medical history. There are very specific markers for diagnosis which doctors use to assess for possible Parkinson’s disease. These markers have a lot to do with a combination of very specific signs and symptoms and if recognised early enough, can be better managed.
1. Primary motor symptoms
- A resti
ng tremor (usually in the hand or foot on one side of the body when a person’s muscles are relaxed and not performing any specific function): A tremor may begin in one finger and typically ceases when a person begins an action or keeps the hand in a flexed grip. Tremors can be triggered or aggravated by excitement or stress. As the disease progresses, so too do tremors, occurring elsewhere in the body, such as a twitching sensation in the limbs. Tremors typically affect one side of the body initially. The most commonly noticed tremor occurs in the hands, fingers or thumbs, but can also occur in the chin or lips. Many develop a pin-rolling tremor which is a back-and-forth rubbing of the forefinger and thumb. For those without Parkinson’s disease, it is fairly normal to experience some shaking at the tail end of vigorous exercise of following injury, as well as a side-effect of some medications. Tremor that is not influenced by these factors and typically occurs during periods of rest may be a sign of possible Parkinson’s disease.
- Slow movement (Bradykinesia): A reduction of spontaneous movement can create an appearance of abnormal stillness, a masked expression, as well as affect speech. Bradykinesia can lead to a decreased ability to perform basic daily tasks such as dressing, using cutlery or brushing hair and teeth. As the condition progresses difficulties with repetitive movements, like tapping fingers, or developing a shuffle when walking, as well as a limited range of movement can also occur. Speech may become softer and muffled, making audibility difficult for others (due to poor enunciation). Speech may also become monotone, losing normal inflections and attributes. Some may experience vocal changes in that they become a little hoarse when speaking. If there have been no recent experiences with viral illnesses which can affect a person’s voice, sudden unexplained changes could indicate Parkinson’s disease. Body stiffness that does not ease with movement, especially in the limbs, shoulders, trunk or hips may be another sign. A person may develop a ‘stiff’ look and not swing their arms naturally when walking. Some also begin to shuffle their feet and do not lift them very high when walking.
- Rigidity and inflexibility: Stiffness in the neck, trunk and limbs is most common. Muscle tone becomes rigid on a more constant basis (muscles do not stretch normally when moving and relax again when resting), which leads to a decreased range in motion. Stiffness can become increasingly uncomfortable, even painful.
- Postural instability and retropulsion: When standing upright, a person may become involuntarily unstable due to a loss of reflexes needed for maintaining posture. A person may easily fall backwards or develop a tendency to sway, especially when standing, turning (pivoting or making other quick movements) or rising from a seated position.
2. Secondary motor symptoms
Other motor symptoms include:
Freezing of gait: Hesitation when stepping forward is a temporary sensation, but common for Parkinson’s sufferers. Many describe the sensation as feeling as if their feet are stuck or glued to the floor. Freezing typically affects the first step and is overcome once it is taken. From there a person generally resumes a normal movement stride. Freezing is also common when pivoting or when approaching objects, such as a chair. Many temporarily overcome freezing by taking exaggerated first steps. In severe forms, freezing can render a person incapable of being able to walk, but most often increases a person’s risk of falling forwards. Hesitation can also be noted in speech, where a person takes a little time to respond (speak).
- Micrographia: As Parkinson’s disease progresses, handwriting becomes smaller as a result of increased difficulty with repetitive actions (bradykinesia). If it is noticed that the change is sudden and words look crowded together and letter sizes decreased, it could be a sign to take note of. It is normal for other signs of aging to influence handwriting changes – stiffening of hands and fingers and deteriorating vision can lead to handwriting becoming smaller and even crowded. The thing to note here is a sudden change. Aging influences happen gradually, over time.
- Mask-like expression and flexed posture: The combination of bradykinesia and rigidity can lead to the face becoming less expressive and a decrease in unconscious facial movements. A person experiences a decrease in blinking motion as well, and appears as if they are staring.
- Uncontrollable accelerations: On occasion, movements that are experienced may be too quick instead of slowed down. Uncontrollable accelerations can affect speech, as well as movement. Speech may become excessively quick and also develop a rapid stammer (tachyphemia). Others may experience uncontrollable acceleration when moving, known as festination, which can lead to frequent falls.
Some individuals may also experience the following:
- Hunched over / stooped posture (forward leaning) - When standing, the body may begin to slouch or lean inwards, causing a hunched over appearance.
- Impaired gross motor coordination
- Impaired fine motor dexterity and motor coordination
- Difficulties with swallowing or chewing
- Cramping
- Production of excess saliva (due to reduced swallowing movements) and drooling
- Sexual dysfunction (erectile dysfunction in men)
- Dystonia (involuntary muscle contractions which result in twisting or repetitive movements)
- Akathisia (sense of restlessness and a compelling need to constantly be in motion)
3. Non-motor symptoms
Symptoms that do not involve physical movement or coordination, and often precede motor problems, can include:
- REM behaviour disorder and other sleep disturbances (restlessness or talking during sleep and vivid dreams) - Many experience restlessness while in deep sleep, and sometimes find themselves falling out of bed. Movements that are sudden may signal possible Parkinson’s disease.
- Changes in sense of smell (anosmia) - Deterioration of neurotransmitters can lead to impairment of smell. Certain smells of foodstuffs, such as liquorice, bananas or even dill pickles may become difficult to distinguish. Loss of smell is common when suffering an infection, such as a cold or flu, but typically returns once cleared. Unexplained sense of smell changes should be checked by a medical doctor.
- Constipation - Strained bowel movements on a regular basis could also indicate Parkinson’s disease. It’s important to rule out other common causes such as a lack of fibre or water in the body, or a side-effect of certain medications.
- Bladder / urinary problems (urination frequency or urgency)
- Problems with vision
- Dental issues
- Problematic skin, such as oily patches and flaky yellow or white scales or dandruff
- Cognitive changes, such as difficulties with memory, confusion, attention span, slow thinking capability and sometimes the development of dementia
- Mood disorders, such as anxiety and depression
- Low blood pressure, especially when rising from a seated position (known as orthostatic hypotension) - this can lead to spells of dizziness when rising from a seated position, or fainting. Unexplained low blood pressure experienced on a regular basis will need to be assessed by a medical doctor as soon as possible.
- Problems with weight (gain or loss)
- Increased sweating
- Lethargy and fatigue
- Impulsive behaviours (most often as a side-effect of medications)
- Visual-spatial difficulties (spatial awareness)
It’s important for a doctor to assess a series of symptoms to either make a Parkinson’s disease diagnosis and begin treatment, or rule out other conditions with similar characteristics or symptoms.
Symptoms are initially mild, even if they develop suddenly, and typically affect one side of the body at first.
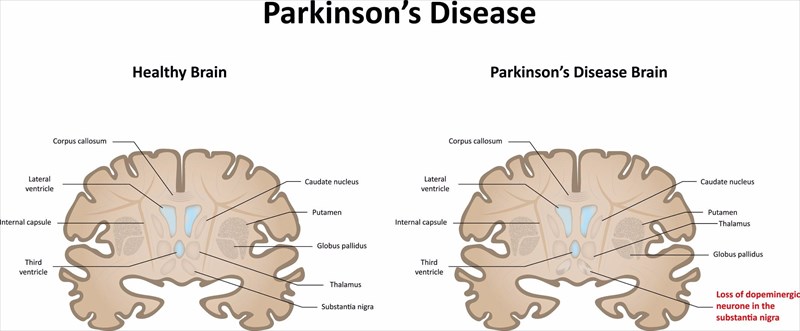
It has been noted by medical professionals that by the time a person generally notices a series of symptoms, dopamine producing cells in the brain would have already affected between 60% to 80% of the neurons needed to maintain and control movement.

 ng tremor
ng tremor Freezing of gait:
Freezing of gait: