How is scoliosis treated?
The treatment options for scoliosis are often complex and each case requires a thorough analysis by a doctor or specialist. There are a number of options for treatment which include braces and several surgical procedures.
The majority of children who have scoliosis tend to have curves that are mild and will not require treatment through bracing or surgery. In these instances, routine check-ups every six months or so are necessary for a doctor to monitor curvature of the spine and whether this progresses or not. The primary treatment for mild scoliosis is observation.
In terms of moderate (25 to 70 degrees) to severe curves (more than 70 degrees)2, treatment commencement and options will depend on the affected individual. There are several factors that a doctor will consider in order to decide whether to treat the condition or wait and monitor it for signs of progression. These include:
- Gender – Females have a higher risk of scoliosis progressing in comparison to their male counterparts.
- Curve severity – The larger the spinal curves, the higher the odds of progression (which will take place over a number of years).
- Curvature pattern – If a double curve, also referred to as an S-shaped curve is present, this will often progress more rapidly and severely than a C-shaped (single) curve.
- Curvature location – A curve located in the thoracic centre of the spine is known to progress and worsen more than curves in the lower and uppers sections of the spine.
- Maturity – As an adult, skeletal maturity is reached and growth stops, lowering the chances of curvature progression. Children who still have some growing left to do have a higher risk of curve progression. As a result, braces tend to be the most effective means of treatment in children who are not yet fully grown.
- Other health conditions – If an affected person has a health concern such as a lung or heart condition and their scoliosis is severe, then immediate treatment may be required so as to limit any complications associated with the rib cage pressing on the heart and lungs.
Predicting the rate of curvature progression
In adolescents and children – Once an abnormal yet mild curvature of the spine has been detected, a doctor will predict whether the condition is likely to progress and become more serious and treat it accordingly.
Progression is purely based on the individual, making it a highly variable aspect and difficult to predict with precision. Three in every 100 adolescents have scoliosis that is severe enough to require at least observation by a doctor2.
Doctors are unable to rely on a definitive risk factor to determine the rate of progression. There is some evidence that suggests that the below-mentioned risk factors can help in determining one’s risk factors:
- Greater curvature angle – An example of how prediction works on the angle of spinal curvature is if the curve is only 20 degrees, then it may only progress by roughly 20 percent. Younger people who are diagnosed with scoliosis and have a 30-degree curve have a higher risk factor as the curve may progress more than 60 percent. If the curve is 50-degrees or more, it may progress more than 90%.
- Spinal issues present at birth – If spinal curvature is the result of congenital scoliosis, then it has a high chance of rapidly progressing.
Curvatures tend to progress at a slower rate in girls who have scoliosis of the lower back and if the spine is out of balance by more than 2.5 centimetres (1 inch)2.
Height also has a role to play. If a girl is shorter than the average height of other girls her age and scoliosis is present in the lower back with an angle of 25 to 35 degrees, she may have little to no risk of progression.
In adults – Some cases of scoliosis that remained undetected or went untreated in youth may develop further and progress into adulthood. The following describes the factors of spinal curvatures in adults and their potential risk of progression:
- Curvatures that are less than 30-degrees are not likely to progress.
- Ways to accurately predict curvature progression of curves that are roughly 40-degrees has not yet been identified.
- Curvatures that are more than 50-degrees have a higher risk of progressing.
Treatment options for scoliosis:
Braces (non-invasive treatment)
Braces are commonly prescribed for children in order to prevent any further curvature progression in curves that are 25 to 40 degrees. Curvature progression in children will be well-documented for reference and monitoring purposes as they grow.
Doctors do not usually prescribe braces for adults with scoliosis due to the fact that this form of treatment is unable to improve the disorder once skeletal maturity is reached. In certain cases, if an adult patient suffers from severe pain, some doctors may recommend a brace as they believe it may able to reduce spinal motion and provide the necessary support to help alleviate pain.
Wearing a brace will not cure scoliosis, nor will it reverse the curvature but it may be able to reduce the rate at which the curve progresses.
The most commonly used braces are made of plastic and contoured to fit the body and conform to it. A brace that is close-fitting around the rib cage, hips, lower back and under the arms can be nearly invisible when worn under clothing.
Options for braces
Generally, there are two different options for scoliosis braces, these include:
- Braces that are worn full-time – Full-time braces are made to be worn for between 16 and 23 hours of the day. The goal is to wear them at all times, except when exercising or bathing.
- Braces worn during the night – Night-time braces make use of hyper-corrective forces, these work by putting the body out of its “normal” balance and cannot be applied when a child is standing or performing daily activities. These braces are worn during the night for roughly eight hours.
Braces will be discontinued once a child’s bones stop growing, this will typically occur:
- Roughly two years after a girl starts menstruating
- When a boy starts shaving daily
- When there are no additional changes to height
When choosing between full-time braces and braces worn during the night, a doctor will look at the location of the spinal curves and what a child prefers. In some cases, night-time braces may be more effective due to the majority of patients being more likely to wear them as this is often more practical and easier to adhere to and helps the sufferer to avoid any associated self-consciousness. Some experts have noted that full-time bracing is more effective, however, this form of bracing is not always as easily accepted among patients.
Currently, experts and medical professionals have not reached a consensus on whether full-time or night-time bracing is best. If the spinal curve is 35-degrees or less, then a doctor may recommend that a child use either a night-time or full-time brace as he or she sees fit. If the curve is 35-degrees or more then a child may be urged to wear a full-time brace.
Other nonsurgical options (these are largely unproven)
The other scoliosis treatments that do not involve surgery may include5:
- Electrical stimulation
- Nutritional supplements
- Chiropractic treatment
- Exercise
Some people claim that treatments like manual manipulation and physical therapy are able to prevent scoliosis from progressing, however, the scientific evidence to back these beliefs is lacking, therefore, these claims cannot be supported. Currently, bracing is the only form of nonsurgical treatment that has proven to reduce spinal curves associated with idiopathic scoliosis from naturally progressing.
This is not to say that these techniques are not helpful to sufferers, however, they cannot stop scoliosis progression.
Some doctors believe that exercise is beneficial to those suffering from scoliosis as it may aid in keeping the back flexible and strong.
When braces fail
In some cases of idiopathic scoliosis, spinal curvature may continue to progress regardless of bracing. Should curvature progress beyond 40 to 50 degrees, surgery might be recommended by a doctor.
A number of adults with scoliosis will not have specific symptoms and will not require any surgical treatment. Because of this, the below section is aimed at children with scoliosis.
The goals of surgery for scoliosis
The surgery for scoliosis will typically have the below-mentioned goals:
- To prevent the curve from progressing – If a child’s doctor recommends surgery, it will be due to the severity of the spinal curve and any associated deformation progressing. Surgery for scoliosis will therefore attempt to prevent worsening of the curve.
- To reduce deformity of the spine – A doctor will evaluate a child’s spinal flexibility as the surgery for scoliosis can untwist any abnormal rotation of the spine and also correct any lateral curvature by roughly 50 to 70 percent. These changes may enable a child to stand up straighter and reduce the rib hump on their back.
- To maintain the trunk balance – If any changes need to be made to the positioning of the spine, then the surgeon will consider a child’s overall trunk (torso) balance and attempt to maintain some of the spine’s natural lordosis and kyphosis curvature. At the same time, he/she will also attempt to keep the legs and hips as even as possible.
Before making adjustments to the spine, the surgeon will consider the effects these will have on a child’s spinal cord. The health of the spinal cord will need to be monitored throughout the scoliosis surgery. The spinal cord is the road for connecting information from the brain and the nervous system, and any injury or trauma to this can result in severe complications that will have an impact on daily life and physical activities.
Surgical options for idiopathic scoliosis
Generally, there are three categories when it comes to surgery for scoliosis, these include:
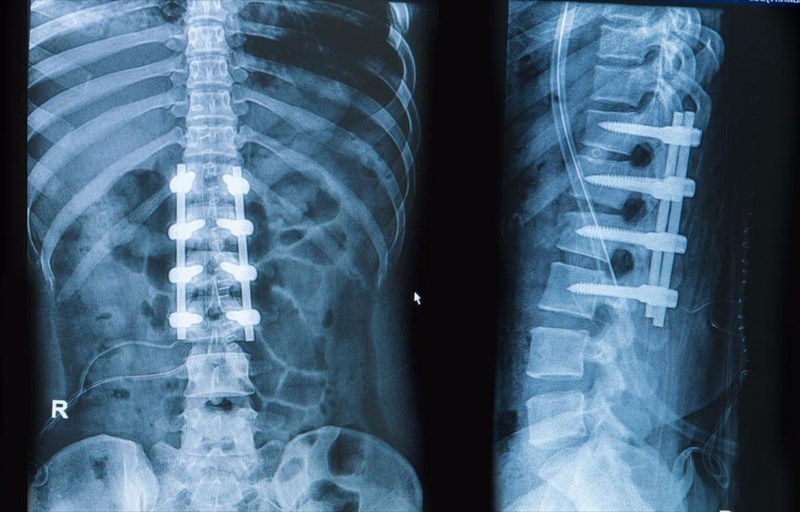
- Fusion – This form of spinal surgery involves permanently fusing two or more vertebrae that are adjacent to each other so as to allow for them to grow together at a spinal joint and therefore, create a solid immobile
There are a number of modern approaches to this surgery which involve instrumentation such as screws, hooks, rods or wires that are placed within the spine to allow for a more efficient curvature correction to be achieved as well as a faster recovery time.
The different methods of spinal fusion include:
- Taking bone from the pelvis or from a bone bank and using this to create a bridge between adjacent vertebrae. This bone graft will assist new bone to grow.
- Using a metal implant to hold adjacent vertebrae together, this will then be removed when new bone has grown between them.
Spinal fusion is a major surgery and tends to last several hours. One of the main advantages of having spinal surgery is that it has a long-term record of efficacy and safety in the treatment of scoliosis. The drawback of spinal surgery is that a child is exposed to post-surgical risks such as infection and may lose mobility and have their twisting and bending capabilities limited. However, with today’s medical advances, surgeons are able to fuse fewer vertebrae together and thus greater mobility can be retained in comparison to surgeries conducted in the past.
- Growing systems – This form of surgery is intended to delay spinal fusion. Growing systems are used in children who have rapidly progressive scoliosis at an early age. A growing rod with an adjustable length is implanted in an initial surgery and then lengthened by means of additional procedures every six to 12 months as a child continues to grow. When the child is closer to skeletal maturity, a doctor may then suggest that he or she has a spinal fusion conducted (if necessary).
When a spinal fusion is done at a very young age (this is typically when a girl is younger than ten years old and a boy is younger than 12), this may result in less room being left for the lungs to fully develop and leave the child with a shorter trunk in comparison to their limbs. In order for these complications to be avoided, a growing system will aid in guiding spinal growth and prevent a curve from progressing as the spine reaches maturity and eventually becomes ready for a spinal fusion (if need be). - Fusionless (Vertebral Body Tethering (VBT)) – There are currently methods that involve applying constant pressure to a bone, which, in theory, will allow for it to grow denser and more slowly. When an outward curvature of the spine is present, a surgeon will attempt to slow down or block the curve’s growth by applying pressure to the outer side, while the inner side of the curve will continue to grow as usual. This allows for the spine to straighten over time. VBT specifically involves growth modulation and aims to preserve flexibility and growth through placing screws on the curve’s outer side and then tightening them through the use of a cord so as to straighten the spine.
Bear in mind, this approach is still a new one and requires additional research and findings in order for the benefits and safety aspects to be explored in more detail.
In the case of adolescents or young adults, spinal fusion remains the preferred scoliosis surgery recommendation.
Choosing surgery or braces
The below-mentioned criteria are generally used in determining whether a person affected by scoliosis should receive a brace, surgery or conservative treatments2:
- Braces are often used for children whose curvatures are between 25 and 40 degrees and where the child still has some significant growing to do.
- Surgery will be suggested if a child’s curvature is more than 50 degrees and he/she has not been previously treated for the condition or if a brace was ineffective. In adults, scoliosis does not generally progress to more than 40 degrees, however, surgery is sometimes an option if a severe amount of pain is present or if scoliosis results in neurological issues.
Bear in mind, that the choice between these options is not always straightforward and some specific cases will need to be further investigated in order to identify the most effective treatment options.
What types of specialists treat scoliosis?
A general practitioner or paediatric physician will typically notice any spinal issues initially, after which, he or she will consult with an orthopaedic surgeon or a neurosurgeon who specialises in spinal surgery. In addition to these specialists, a rehabilitation expert or a physical therapist may also be consulted.
Some people may require an occupational therapist or a neurologist to be a part of their treatment team on an ongoing basis. An occupational therapist aids in helping one to adapt to any physical incapability’s that may develop as a result of the condition or when recovering from surgery.
References:
2. University of Maryland Medical Centre. 2012. Scoliosis. Available:http://www.umm.edu/health/medical/reports/articles/scoliosis [Accessed 07.09.2017]
5. Niams. 2002. Scoliosis in children and adolescents. Available: https://www.niams.nih.gov/health-topics/scoliosis [Accessed 06.09.2017]
