Signs and symptoms of smallpox
Indications of a smallpox infection typically presented symptoms in stages:
1. The incubation stage
At this stage, a person had contracted the virus (via the respiratory tract) but did not yet feel ill. During the incubation period, a person was thus typically asymptomatic and would not likely be aware of infection.
Within the initial 72 hours, VARV began to infect the body’s white blood cells (macrophages). It then began to move and multiply affecting the lymph nodes. From there, the virus proliferated further, reaching the spleen and bone marrow. Once the virus re-entered the bloodstream (via cells known as leukocytes), the first symptoms (normally a high fever) typically developed.
As the virus circulated within the body, infected structures (like the bone marrow, spleen, liver, kidneys and lymph nodes etc) took on large quantities of the virus.
As no symptoms had yet developed within 7 to 17 (sometimes up to 19) days, a person was not yet contagious (i.e. could not yet transmit the disease / pass on to another person).
2. Early signs and symptoms (prodromal phase)
Following the incubation period, initial symptoms developed, lasting between 2 and 4 days. These included:
- A high fever (38.8-40°C or between 101-104°F)
- Headache (this could be severe)
- Body aches (including backache / spinal pain)
- Body weakness
- A sore throat (pharyngitis)
- Mouth ulcers
- Nausea
- Vomiting (this could be occasional and did not affect all infected individuals)
Not everyone was contagious at this early stage of infection. It was only really during the following symptoms stages that a person became a risk around others. A person did, however, begin to feel very sickly and may not have been able to function as normal.
While rare, the following symptoms were also recorded:
- Delirium
- Depression / psychosis and manic depression
- Hallucinations
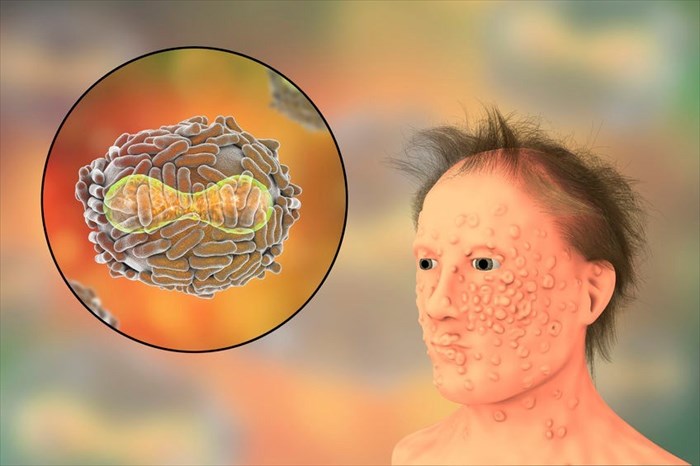
3. The characteristic rash
After the fourth day of ill health, skin lesions or bumps became noticeable on the surface of the skin as a rash developed, as well as a continued fever. The development of the rash generally took place over a 4-day period. At this stage, a person was at their most contagious and could spread the virus.
- The initial stages of the rash presented as small, red spots, accompanied by the development of ulcers in the mouth and on the tongue. Fever began to decline a little, alleviating some of feelings of illness.
- The small spots developed into slightly larger sores (round lesions or bumps known as papules), becoming firmer (or cyst-like) and filling with (thick) fluid.
- The lesions often appeared to have a small dent / depression in the centre of each sore. These sores tended to break open, spreading fluid that contained VARV further into the mouth and throat.
- The rash / sores then typically spread to the surface of the skin, most often affecting the face first, followed by the limbs (arms and legs), hands (and palms), feet (and soles) and trunk. Once this happened, the remainder of the body began to break out in sores within 24 hours.
- The infected person often developed a high fever once more, which typically remained until each lesion or sore developed a scab.
Pustular rash and scabbing
By the 5th or 6th day the rash sores / bumps had developed into larger pustules (i.e. sores filled with a cloudy fluid or pus). The pustules looked like raised white bumps (which were almost pimple-like in appearance) surrounded by inflamed skin (erythema or redness). Each pustule felt firm to the touch.
Between day 6 and 10, each pustule developed a crust or scab. The majority of pustules formed a scab by about the 14th day. The infected person was still very much contagious while the pustules scabbed over.
Within the following 6 days, the scabs began to fall off the rash pustules (this was known as shedding), leaving pitted scars on the skin’s surface. The entire formation of the rash / pustule lesions and scabbing process could take as long as 3 to 4 weeks in total before all scabs had been shed from the body.
Once all scabs had fallen away, the infected person was no longer considered contagious.
Symptom distinction by major VARV sub-type (*based on observations before the eradication of smallpox)
1. Ordinary smallpox
- Sudden onset of a high fever
- Severe headache
- Body aches (particularly backache)
- Vomiting
- Diarrhoea
- Rash (distribution patterns: confluent – mostly on the face and limbs, semi-confluent – mostly present on the facial area and discrete portions of skin or discrete – affecting areas of skin between pustule formations) – lesions / sores are deep-seated, round, firm and range from a few to several thousand.
2. Modified smallpox
- Similar symptoms to ordinary sub-types
- The exception occurred in the rash formation – this developed a little more quickly but with smaller sized pustular lesions.
3. Malignant / flat smallpox
- Pustule formations were flat with confluent or semi-confluent distribution patterns (more common in children).
4. Haemorrhagic / fulminant smallpox (sometimes referred to as ‘sledgehammer smallpox’)
- Skin lesions / pustules and mucous membranes broke open (i.e. haemorrhaged)
- Extreme physical weakness, heart failure, bone marrow suppression and diffuse bleeding were complications which could arise, making a person’s condition life-threatening. Complications could also arise due to secondary bacterial infections.
5. Variola sine eruptione (variola sine exanthemata)
- Fever
- No rash
How common is smallpox?
Smallpox was a fairly common disease before the successful implementation of a global eradication programme initiated by the World Health Organization (WHO) in 1959. Infections occurred in individual of both genders and at any age. The programme was intensified due to a high number outbreaks and widespread infections, offering routine vaccinations during the late 1960s.
By the mid to late 1970s, the programme had been able to successfully eradicate the disease in many countries. On 8 May 1980, the WHO released an official statement declaring the world free of the smallpox disease with no further reported cases of natural infections occurring anywhere in the world. (6)
The last endemic case of major VARV infection was recorded in Bangladesh in 1975. The last minor VARV endemic case is recorded as having occurred in Somalia in 1977. A laboratory accident in Birmingham, UK too place in 1978, infecting one person.
Reference:
6. Centers for Disease Control and Prevention. August 2016. History of Smallpox: https://www.cdc.gov/smallpox/history/history.html Accessed 06.04.2018]