- Spinal stenosis
- What causes spinal stenosis?
- Location and types of spinal stenosis
- How does spinal stenosis affect the body?
- Who is at higher risk of developing spinal stenosis?
- How is spinal stenosis diagnosed?
- What is the treatment for spinal stenosis?
- Coping with spinal stenosis
- What is the outlook for someone with spinal stenosis?
Location and types of spinal stenosis
Spinal stenosis is classified medically in two ways:
- According to aetiology, i.e. whether it is primary (congenital/developmental) or secondary (degenerative/acquired).
- Based on the location of the condition within the spine and the precise area in which the neural structures (spinal cord and/or nerves) are affected.
Compression or constriction of the spinal cord and nerves can occur at any point along the spinal canal. Symptoms which develop are determined by the anatomical location and type of stenosis present. The most common areas where stenosis occurs are the cervical and lumbar portions of the spine (i.e. the neck and lower back). However, it is possible for a person to experience narrowing in more than one location along the spine, and thus have more than one type of stenosis.
To determine the location of stenosis and the possible underlying cause, a medical doctor must evaluate a patient through a physical exam and appropriate testing. In so doing, appropriate treatment can be recommended.
Location of the constriction or compression can occur in the following anatomical regions of the spine:
1. Lumbar spine (lower back)
The most common type of spinal stenosis occurs in the lumbar area of the spine (L1 through L5 vertebrae) and is therefore referred to as lumbar stenosis, and more often than not is due to the degeneration of connective tissues (muscles and ligaments), discs and vertebrae. Stenosis in this area of the body leads to leg pain and walking difficulties (or pain with activity). Pain may radiate from the lower back into the buttock area and legs, most especially when a person is active (i.e. moving around – walking, dancing, exercising).
The most common reason for lumbar spinal stenosis is degeneration associated with aging. The facet joints which stabilise the vertebrae, enlarge and compress the spinal nerve roots in the lower back. A spinal injury or curvature of the spinal canal in younger individuals can also lead to the development of lumbar spinal stenosis, although this is rare.
A person with lumbar spinal stenosis typically feels more comfortable while in seated positions, and more uncomfortable when upright and moving (and may experience claudication – leg pain with movement, such as walking). Many describe the onset of pain as being experienced in the legs, and report weakness in the limbs. Some find relief by walking in a forward flexed position (i.e. leaning forward on something like a shopping cart, trolley or walker / Zimmer frame), or when in a sitting position.
Standing in an upright position decreases the space between the nerve roots and vertebrae, effectively blocking blood flow around the nerve. This causes blood to become constricted and irritates the nerve, resulting in symptoms of discomfort and pain. Over time this can lead to severe nerve damage (affecting vertebral segments, which together are referred to as a degenerative cascade), and is best prevented or treated with surgery.
During the earlier stages of the condition, changes in fine motor skills and coordination, as well as balance, and the development of numbness, tingling and weakness (i.e. symptoms of sciatica) in the limbs, may be noted.
Lumbar spinal stenosis can sometimes mimic the symptoms of vascular insufficiency (an impaired functionality of vein valves in the legs, resulting in swelling and skin problems such as discolouration and ulceration).
2. Cervical (neck)
Compression and narrowing occurs in the neck area of the cervical spinal canal (vertebrae C1 through C7) and is referred to as cervical stenosis or cervical spinal stenosis. This is most often as a result of traumatic injury or degenerative changes (natural wear and tear) which occurs gradually over time. Neurological problems (also known as myelopathy), such as pain, weakness, numbness and a loss of limb coordination develop as a result of this compression. Pain and other symptoms may radiate to the arms and hands. When stenosis is accompanied by symptoms of myelopathy (compression of the cervical spinal cord), a diagnosis of cervical spondylosis with myelopathy (also known as cervical spondylotic myelopathy) will likely be made.
Stenosis merely refers to the narrowing or compression which takes place at a point alone the spinal canal. Spondylosis refers to the resulting degeneration which causes symptoms.
When intervertebral discs begin naturally losing hydration as the body ages, they become flatter, and can bulge into the spinal canal. Facet joints (those at the back of the spine) can also degenerate with age and hence enlarge, most often due to inflammatory conditions such as arthritis. Degeneration of these discs and joints can result in spinal stenosis. Herniated discs (pinched nerves and bulges), bone spurs (bony projections which occur along bone edges), and swollen ligaments can also all lead to cervical stenosis / cervical spondylosis with myelopathy.
Symptom progression of cervical stenosis is not always a predictable pattern. and can vary from one person to the next. Symptoms can remain the same (‘stable’) for long periods of time or rapidly worsen. In general, symptom progression tends to worsen at a gradual pace.
Non-surgical treatments for cervical stenosis are generally considered when myelopathy symptoms are characterised as reasonably mild (usually during earlier stages). In most cases however, pressure on the spinal cord is relieved surgically. Surgery is a preferred means of treatment due to the severe risk of nerve damage which can occur as the condition progresses.
3. Thoracic (mid back)
Thoracic stenosis occurs along the upper / middle portion of the spine, mainly affecting the vertebrae and spinal nerves connected to the rib cage (T1 through T12). However, this portion of the spine requires less movement and is generally more stable and stronger than its cervical and lumbar counterparts. As such, degeneration due to compression occurs very rarely in this area.
Types of spinal stenosis
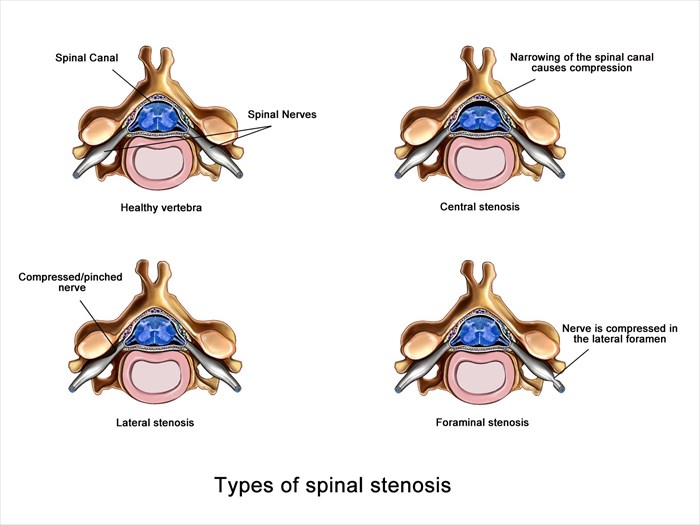
The types of spinal stenosis are classified according to the specific place within the vertebra/e that the neural structure (i.e. either the spinal cord or spinal nerve root) is affected as follows:
- Lateral stenosis: This occurs in the tract where the nerve root exits the central spinal canal, known as the lateral recess. Depending on the anatomical location of lateral stenosis, it will be referred to as either lateral cervical stenosis, lateral thoracic stenosis or lateral lumbar stenosis.
- Central stenosis: This condition occurs in the central spinal canal and may place pressure on the spinal cord or cauda equina nerve roots. In reference to where this type of stenosis occurs within the spine, it will be termed either central cervical stenosis, central thoracic stenosis or central lumbar stenosis.
- Foraminal stenosis: This type of stenosis occurs in the lateral foramen (passage-like openings on either side of the vertebra) where nerve roots branch out of the spine to the rest of the body. Based on the anatomical location of this type of stenosis within the spin, the condition may be diagnosed as either cervical foraminal stenosis, thoracic foraminal stenosis or lumbar foraminal stenosis.
A wait and see approach is not recommended when symptoms of spinal stenosis first appear. As compression worsens, more pressure develops and symptoms become more severe. This can result in paralysis in one or more limbs (arms and legs), and have a domino effect, impairing other bodily functions too.